
New generations of precision digital scanners are threatening to replace the tool that has been the iconic symbol of pathology for so long. Maria Delaney reports.
Glass slides containing tissues and cells are sitting in piles on a shelf in the pathology lab. They wait here until the consultant picks up a stack and carries them to a microscope for analysis. An analogue system in a digital world.
Well that’s how Michael McKenna sees it. He is clinical lead for pathology services in Altnagelvin Hospital, Northern Ireland, and wants to move their system from slides to screens. “We want to report off the screen because this makes it more efficient and productive,” says McKenna, who is currently trying to find a mechanism to scan slides and report them through their existing picture archiving and communication (PAC) system.
There are a number of pathology labs in Europe that have already gone digital. LabPON, a large pathology lab in the Netherlands, is one such early adopter. Linköping Hospital in central Sweden is another.
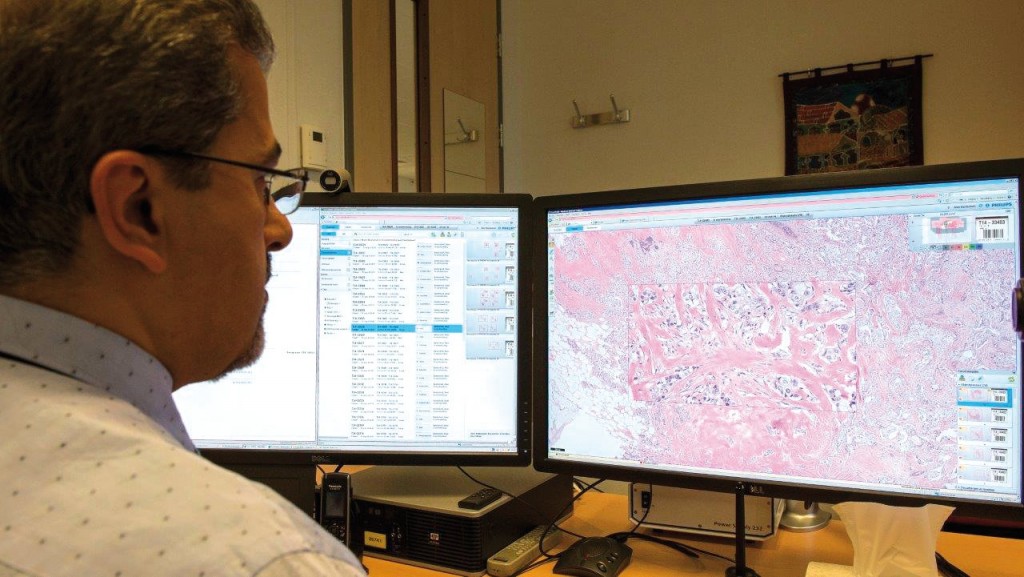
Three years ago all of the histology samples at Linköping were digitised, and they now scan just under 200,000 slides every year. Instead of looking at slides through a microscope, Arrigo Capitanio, consultant pathologist at the hospital, analyses scans of the slides on a high-resolution screen.
He notes that many fields have improved with digitisation and feels that the same is true for pathology. “A trainee in radiology can’t imagine that all the instruments they are currently using didn’t exist just 30 years ago,” he says.
Linköping has six slide scanners: four for clinical slides, one for large histological sections, and one dedicated to research. They run day and night to allow almost real-time scanning. A variety of suppliers are involved, including Hamamatsu and Aperio for the scanners, as well as SECTRA for the digital platform/viewer.
One of the biggest benefits to working digitally, says Capitanio, is that he can “ask a colleague in New York by email or Skype to look at the slide and discuss the case”. This means pathologists can get much greater access to expert opinion without having to delay their report.
Without a scanner, obtaining a second opinion takes much longer. First you write an email or letter to the relevant colleague, then you post the slides. Capitanio remembers hoping that the slides would not be broken when they arrived. Other hazards include the slide being delayed en-route or sometimes disappearing on its return journey. “It’s quite a big difference,” he says.
At Altnagelvin Hospital, the PACS system for radiology was implemented as part of a huge project that involved two datacentres and 27 hospitals across Northern Ireland (NI). Known as NIPACS, and using a platform developed by SECTRA, the system not only digitised radiology requests and consultations within each hospital, but also linked all the hospitals within the system. Brendan Devlin, radiologist at Altnagelvin, was one of the driving forces behind its implementation.
Shortly after getting the system, Devlin remembers sitting at his desk and receiving a message from his colleague in a hospital 100 kilometres away. “He was asking me to give a second opinion on a CT liver and since the message is automatically linked to the examination, within a few minutes I was able to send a message back.” Before NIPACS this type of request would have taken days or weeks, says Devlin. “It’s all to do with speed, efficiency and quality.”
Devlin, who now also works with SECTRA to promote digital platforms, believes that “all medical images should be treated with the same robust storage and sharing facilities,” and says NIPACS can offer that. As he points out, pathology is just one area producing images. Others include medical photography, diabetic retinopathy, dermatology, cardiology, and ultrasound.
Closer scrutiny
When pathology joins radiology on NIPACS in Altnagelvin, Devlin feels it will be the quality of scrutiny the report receives at the multidisciplinary team meeting where the real impact will be felt. “It revolutionises them in terms of an effective discussion of the patient’s case,” he says, because, if all the images are available, the team gets the opportunity to interrogate and confront.
Devlin himself likes to be challenged and forced to justify what he’s written, which he sees as a matter of quality assurance. “It’s not just a question of reading my report,” he says.
This has certainly been the experience at the LabPON pathology labs in the Netherlands, according to Alexi Baidoshvili, pathologist and project director of the digital pathology team. Multidisciplinary team meetings, he says, work much better when digital files are used. Other advantages he lists include faster consultation, the ability to compare a number of slides, a cleaner work environment, and better logistics.
Notable by its absence from that list, however, is the quality of the images themselves, which Baidoshvili argues is not quite as good as microscopy. “It’s always a choice,” he says, arguing that the marginally poorer quality is more than compensated for by the improvements in the diagnosis process and logistics. The problem will be solved in the near future, he says, as “scanners become better every year.”
Capitanio denies there is a problem at all. The important point is to be able to recognise the subject, he says. He uses George Clooney and Naomi Campbell as examples, asking whether it is easier to recognise them in person or by looking at a photo.
The tissues and the changes present in the histological preparation can be recognised perfectly in a good-quality scan, he says. “In other words: it is diagnostic.”
NIPACS: a national virtual department
One of the largest RIS/PACS (radiology information system/picture archive and communication system) projects ever undertaken worldwide was conducted in Northern Ireland, where 27 hospitals were connected by a system called NIPACS.
Provided by SECTRA, this digital platform caters for more than 1.4 million patient examinations a year. All radiology images captured in the participating hospitals are stored in a central archive in Belfast.
The vision of NIPACS includes a virtual radiology department across Northern Ireland, full availability of images and reports, a system to revolutionise dispersed networked care and minimisation of training issues and clinical risk.
The assignment of a unique “Health & Care” number to every individual in Northern Ireland was a key factor supporting its implementation, says Brendan Devlin, former lead radiologist of NIPACS. “Robust identification is the cornerstone of these integrated systems because you can’t afford to put the wrong images in the wrong place,” he says, pointing in particular to the huge medico-legal implications.
The NIPACS service was launched in 2009 after many years’ preparation. The new technology costs £31mn (€40mn) over 10 years.
Making the change
Implementing major change to complex procedures rarely goes smoothly, particularly when IT systems are involved. Capitanio, in Sweden, says the main problem in his lab was the transition from the microscope to the computer for the pathologists. “Some simply don’t want to do it.”
The turning point for many came when they experimented with the digital system. “Colleagues who were sceptical at the beginning now work very well digitally, and some also became quite enthusiastic,” he says, though he adds that some are sticking with the “glasses” (glass slides).
This works in Linköping, as the pathologists receive both the digital and glass slides for analysis, which Capitanio says is needed, because in around 3% of digital slides the scan is not perfectly in focus, despite the quality control. “Rather than send everything back, I look at the microscope, because there is a turnaround time to respect,” he says.
At his hospital, the change to digital also required a major reorganisation of the whole histology lab to standardise the method of production needed to produce high-quality scanned images. Some of the practical problems Linköping encountered were coverslip precision, drying of the slides before scanning and, for smaller histology blocks, correct positioning of the section on the slide.
McKenna in Northern Ireland says he does not expect such a major reorganisation will be needed at the Altnagelvin pathology lab, because it already functions in a very linear fashion, so it should be simple to add a scanning step at the end of their current method. The lab is also based in a new building within the hospital, which has space for new machines. When it was originally designed, the pathologist explains, “they already knew that technology was advancing and a lot of the things that we normally did manually would be replaced by technology platforms, which tend to have quite a substantial footprint compared to a human.”
McKenna points to a corner of the lab where the slides are currently stacked, to show where he intends to locate the machines he will need. But he recognises that not all labs have been built with new technology in mind, and this could pose a problem. “Some labs will need to invest in infrastructure if their building is too small,” he says, in which case, “it’s not just about procuring a piece of equipment, it’s also about knocking down a wall or building an extension.”
Getting to grips with the require-ments of digital technology can also be a bit of a learning curve, according Baidoshvili, who says they have had to change the server at LabPON three times since the system went live last July. “Every time we use more scanners, or more pathologists start with digital diagnosis, the server becomes slow,” he says.
Currently they use four scanners, as well as two backup scanners, and process 300,000 slides per year. They are using the Philips Digital Pathology Solution for both their scanners and digital platform/viewer.
The changes in working practices also brought new work-related health hazards, with some pathologists developing repetitive strain injury – inflammation in the arm and shoulder – from spending all day moving images around with a mouse.
Baidoshvili notes that using a microscope all day is also known to cause problems, but he didn’t want to create new problems with digitisation. Working in partnership with Philips, they created additional user interfaces, such as a touchpad, and Baidoshvili says that he now protects himself from RSI by alternating between devices over the course of a day and also using both hands.
Devlin recognises the problem and says ergonomics was also an important issue in the Northern Ireland project. He sits at a work station that can tilt and be raised or lowered to suit him, and he uses an ergonomic multi-button mouse to control the PACS and minimise use of the keyboard.
“You’re not uncomfortable, you’re not distracted,” says Devlin. His own work station is in a dark room with wall panels to muffle sound. A number of work stations are also housed in a communal reporting room for easier communication with colleagues and to facilitate second opinions. “It’s all part of better quality,” he says.
As far as McKenna is concerned, the switch to digital can’t come fast enough. He is looking forward, above all, to moving from Vernier scales on a microscope to clicking a mouse. Measurement is really “tiresome and cumbersome” at the moment, he explains. “With a digital image, the ruler is there and you just pull it from point to point.” This is not only easier, he says, but also improves accuracy and enables pathologists to leave a record of the measurement.
A resource for research
In addition to the clinical applications of digital pathology, slides are currently being scanned for research purposes. The European Organisation for Research and Treatment of Cancer (EORTC) has a number of projects which are doing just that.
Pathology review for the INNOVATION trial (http://tinyurl.com/eortc-innovation), includes scoring tumour regression after neoadjuvant treatment of HER-2 positive, resectable gastric cancer. This will be done using scanned slides which will be viewable by the review panel members via the Internet.
The EVIDENCE trial (http://tinyurl.com/eortc-evidence) will scan the slides for quantitative, digital assessment to calculate the percentage of residual viable tumour cells at the site of the primary lesion in early-stage non-small-cell lung cancer.
The EORTC is also planning to set up a digital platform for review of scanned slides as part of their new Screening Patients for Efficient Clinical Trial Access (SPECTA) programme. Edit Szepessy, a translational researcher at the EORTC, says this will be particularly valuable for their thoracic and rare cancers projects: SPECTAlung and SPECTArare.
Digital futures
Digital pathology in Linköping and LabPON is only for histology to date. As Capitanio explains, this is because the tissue or tumour section lies on the glass, so single-level scanning with a focus depth of about one micron is enough for this type of specimen.
Cytology samples, by contrast, are made up of cells from fluids such as urine or sputum, or from the abdominal cavity or around the lungs. Micro-focusing is needed to analyse these cells, which involves changing the focus level, second by second, to see different levels in the slides. “To do this digitally, it is necessary to scan several levels and then to use software to see all these levels,” says Capitanio. This consumes a lot of time and data, so it cannot be used for routine diagnosis with current technology.
Cytology samples are, however, already being scanned at Linköping for the purposes of teaching, documentation and research. A number of companies are working on new types of scanners that can do this automatically.
Arguments for cost saving with digitisation mainly involve process improvements for the pathologists, rather than reducing workload in the lab. In fact scanning is an extra step on top of the normal slide-making process. This is in contrast to radiology, which can remove the film-making process and associated costs when moving to digital images.
One cost saving that falls outside of the norm is storage. “You don’t have to store the glass slide because, if you scan the image, the image is stored for as long as legally required,” says McKenna. This means the glass slide could be disposed of after a shorter period of time.
This saves money, as the cost to store the glass slides “is increasing every day,” according to Capitanio, whereas digital storage costs are reducing. In his previous job at University College London Hospitals, costs for storage were so high that the slides were sent on a lorry to Wales.
There are many arguments and lines of thought about the future of pathology, but why should labs move from microscopes to screens? Capitanio has a simple answer. “Why not? We’re in the digital era.”
For Baidoshvili, the question is already out of date. His focus is on where digital pathology is going next. His first goal is to become completely digital, including cytology, he says. When that is accomplished, the plan is to focus on image analysis, which Baidoshvili says is the future of pathology.
He is collaborating with other labs in the Netherlands, as well academic hospitals and Philips, to create software to use in their daily diagnostics. This will make their work much faster and more accurate, according to the digital enthusiast.
Back in Northern Ireland, McKenna sits back at his desk with a microscope on one side and a computer on the other. Glass slides in position and ruler in hand, he turns to the analogue machine. Perhaps not for much longer.




