By the time they reach 40, survivors of childhood cancers are likely to have at least one chronic health problem resulting from their treatment. The search is now on for ways to help people manage their risk and get appropriate care.
 Childhood cancer may be rare, but survivors are not. One of the big success stories in oncology has been the steadily increasing proportion of children and young people who survive to adulthood, and who now number in the hundreds of thousands in Europe. The latest EUROCARE-5 study shows an average five-year survival of 79% for children aged 0–14 (five-year survival is currently around 60% in Europe and the US).
Childhood cancer may be rare, but survivors are not. One of the big success stories in oncology has been the steadily increasing proportion of children and young people who survive to adulthood, and who now number in the hundreds of thousands in Europe. The latest EUROCARE-5 study shows an average five-year survival of 79% for children aged 0–14 (five-year survival is currently around 60% in Europe and the US).
Survival in the teenage and young adult age group – 15–24 years old – is also similar to children, although there are differences in outcomes for certain cancers such as leukaemias and central nervous system tumours. There are also differences between eastern and western Europe, but the greatest gains recently have been in the east, where five-year survival has risen from about 65% in 1999–2001 to over 70% in 2005–2007 in the 0–14 age group.
But the mostly good news is offset by problems that are common in adult survivors of childhood cancers, who now greatly outnumber those currently undergoing primary treatment. While there is no definite number of adult survivors of childhood cancers in Europe, experts say it is at least 300,000 and could be as many as 500,000 people, and the current survival statistics translate into about 10,000 a year being added to this growing group. It’s a similar picture to the US, where adult survivors (who were diagnosed with cancer aged 20 or under) are estimated to number more than 400,000, and are set to reach half a million by 2020, with an annual incidence of new cases of about 13,500 a year.
According to the authors of a recent paper in Nature Reviews Cancer (2014, 14:61–70), this growing population “reflects a highly vulnerable group of individuals who will probably experience adverse health-related and quality of life outcomes during their subsequent lifetimes as a result of their curative cancer treatment.” The vast majority, the authors say, will have at least one chronic health condition by the age of 40, and there is a high risk of early death from subsequent cancers and heart and pulmonary conditions. While there can be multiple causes of later ill health, most survivors suffer only because of the late effects of certain treatments for their childhood cancer.
So a priority for healthcare systems should be to characterise those survivors at highest risk and offer them interventions for late effects, which can be caused by all types of treatment – surgery as well as chemo- and radiotherapy – and also to offer help with psychosocial and quality of life issues. There are many late effects that survivors can suffer from, but most people have little long-term follow-up and guidance after they ‘transition’ into the world of adult healthcare, where most professionals lack experience of these effects. This means improving the care of survivors is a big challenge.
This challenge is now being tackled by several groups around the world, not least by PanCare, the Pan-European Network for Care of Survivors after Child and Adolescent Cancer. PanCare was set up in 2008 by paediatric oncologists, other medical specialists, epidemiologists, nurses, parents and survivors, to carry out research and develop guidelines on late effects, with the eventual aim of ensuring every child and adolescent survivor receives optimal long-term care.
The survivorship passport
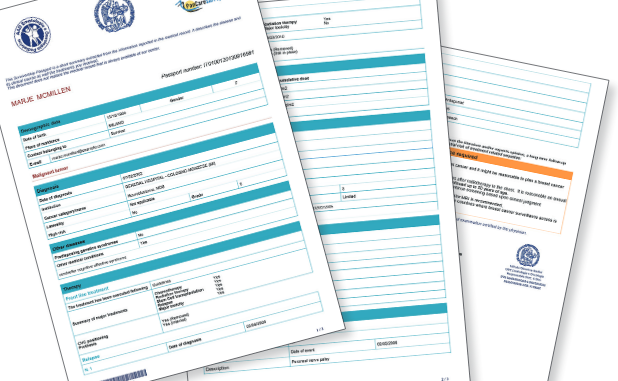
The group has had notable success so far. One advance came when it was asked by the European Society of Paediatric Oncology to develop a survivorship work package in the European Network for Cancer Research in Children and Adolescents project, funded by the EU Framework programme. This package focuses on quality of survivorship, and a key part is the introduction of a survivorship ‘passport’ – a summary of medical history that could give people much better follow-up treatment as adults.
Riccardo Haupt, one of PanCare’s founders and a paediatric oncologist and epidemiologist at the Giannina Gaslini Institute in Genoa, Italy, is the lead on the passport, which he says was lobbied for by parent associations and survivors in the PanCare network. “We know from them that many people lose contact with their cancer centre and do not have documentation on their treatment,” he says. “They also often have trouble discussing problems with their GP or with specialists such as cardiologists, who may say, ‘You’ve had cancer – I’m not an expert in this.’”
The passport aims to provide vital data on previous treatment and recommendations on follow-up for late effects for each patient. The first step has been to generate the list of variables that are important for survivors, such as tumour type, risk factors, treatment exposure and so on, which was settled via a Europe-wide ballot. “The second step is to see how complicated it is to complete the passport by inserting the data,” says Haupt.
Most cancer centres and hospitals do not have records suitable for filling out the passport data fields, and expecting staff to spend an average of more than two hours gathering medical history for each patient is probably not realistic, adds Haupt. A number of data integration methods are therefore being investigated. One advantage of child patients is that the great majority are treated under trial protocols, so data on diagnosis and treatment can be gathered from clinical trials databases.
Sabine Karner, who had cancer when she was young, and who works for Austria’s childhood cancer advocacy organisation for parents, has been involved with the passport’s development through the International Confederation of Childhood Cancer Parent Organizations, (ICCCPO), which is a member of PanCare, and runs the International Childhood Cancer Survivors Network.
“Paediatric oncologists have listened to the voice of survivors in helping to develop the passport. Many of us simply don’t know our history and the long-term effects we could have, and who we should go to when we have a problem,” she says. “How, for example, do survivors know if something could be connected with their former treatment? And this is a life-long concern.”
Karner points out that some childhood cancer centres, such as the St Anna children’s hospital in Vienna, have already produced versions of passports, mostly only as a paper document. The goal now is for everyone to have a standardised one available both online and as a printed document.
“Of course not everyone needs or wants support, but many are simply lost to contact once they are no longer the responsibility of a children’s hospital,” she says, adding that some countries still have no specialist facilities for older teenagers and young adults with cancer, where the survivorship data could be prepared.
“Many of us simply don’t know our history and who to go to when we have a problem” There are though a growing number of survivor groups around Europe, such as a recently established Les Aguerris group in France. Some are dedicated to survivors, while others are set up as subgroups of organisations for parents of those with children with cancer “These groups will raise awareness – and the passport is now very much on the European agenda,” says Karner.
So far, a prototype of the passport has been developed by Cineca, Italy’s non-profit university computer consortium, with leukaemia patient data from the Italian Association of Paediatric Haematology and Oncology; other groups in Europe are looking at structuring data for neuroblastoma, sarcomas and Wilms’ tumour. Decisions about the coding systems for the passport have been complicated, adds Haupt, such as on whether to use the international childhood codes for tumour types, and how best to code complex radiotherapy information, which could also trigger certain recommendations for follow-up.
And there are privacy and data security issues: “For example, who is the owner? Should only the survivor have access or also their GP?” asks Haupt. While the aim is to empower survivors to be responsible for their long-term care, he adds, it is proving hard to translate medical language, for instance about risk factors, into words that people won’t find too alarming: “Defining the way the information is disseminated has become a project in itself.”
 Guidelines for follow-up and care
Guidelines for follow-up and care
Feeding into the work on the passport is another initiative dedicated to developing guidelines on clinical practice and how the transition to, and follow up in, adult care can best be implemented. Known as “PanCareSurFup” (PanCare Childhood and Adolescent Cancer Survivor Care and Follow-up Studies), the intention is to incorporate the recommendations from the guidelines developed by this project into the survivorship passport.
Guidelines are particularly needed in the wider medical community – such as GPs, cardiologists, endocrinologists, gynaecologists, and indeed for oncologists outside the paediatric field, says Haupt. “We see the guidelines as the key to making contact with these professionals,” he says, adding that this is a global effort from the International Guideline Harmonization Group for Late Effects of Childhood Cancer (www.ighg.org), which was set up in 2010 to bring various groups together, with PanCareSurFup as the guideline development partner. Other core members include the Scottish Intercollegiate Guidelines Network, which published a national guideline on long-term follow-up in 2013, the North American Children’s Oncology Group and the Dutch Childhood Oncology Group.
A first clinical guideline has already been published, on recommendations for breast cancer surveillance for girls and young women who were given chest radiation as part of their treatment for cancers such as Hodgkin’s lymphoma (Lancet Oncology 2013; 14 e621–29). It covers questions such as who needs surveillance, at what age and how frequently. It emphasises how important it is for survivors to be aware of their risk, and makes recommendations for breast cancer surveillance graded according to the amount of radiation that was received. The next topic that will get the guideline harmonisation treatment will be gonadal toxicity.
PanCareSurFup’s work packages also include developing risk estimates for cardiac disease, later cancers and radiation dosimetry for various organs, which will inform other guidelines. Underpinning the project is the inclusion of what Haupt says will be the world’s largest cohort of long-term survivors, 80,000 in total, who will be followed up by 16 networks and institutes around Europe.
Another PanCare project involves identifying possible genetic risk factors for certain late effects – namely fertility problems and hearing loss – and is coordinated by Mainz University Medical Centre in Germany.
Underpinning the project is the inclusion of the world’s largest cohort of long-term survivors, 80,000 in total
The implementation challenge
The projects are important but Haupt and colleagues face the greatest challenge in embedding survivorship care in national health systems, and getting innovations such as the survivorship passport running as widely as possible. It will be easier in countries with integrated national systems, such as the UK (where aftercare ‘pathways’ and pilot projects have been underway) and the Netherlands, but less so where there are fragmented regional systems, such as in Italy, says Haupt.
There is also the need to convince health services to cover the added cost associated, for instance, with introducing interventions such as breast surveillance, which in the long run could reap substantial savings by cutting the burden of chronic disease.
Survivors and health professionals such as nurses also need financial support to maintain networking, says Haupt, while research and follow-up cannot stand still, as today’s treatments will change or be discontinued in favour of new ones, leading to different patterns of long-term effects.
“There is a lot of expectation now among survivors and their families,” says Haupt. “Once it is recognised that this is a population at risk, the recommendations we will be making should be a standard of care in each country.”