According to Kaasa, head of the Cancer Clinic at Trondheim University Hospital, patients are falling through gaps in care provision because palliative care is seen as an add-on rather than integral to care plans.
The World Health Organization has a definition of palliative care, but it is by no means a short one. Yes, it is “an approach that improves the quality of life of patients and their families facing the problem associated with life threatening illness.” But that is just the start. We need to have “early identification and impeccable assessment and treatment of pain and other problems”, integration of “psychological and spiritual aspects of patient care”, “support systems” for patients and their families, and a “team-based approach”.
A crucial part of the definition, as Stein Kaasa, a palliative care expert and head of the Cancer Clinic at Trondheim University Hospital (St Olavs)in Norway affirms, is the last point: “It is applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life, such as chemotherapy or radiation therapy, and includes those investigations needed to better understand and manage distressing clinical complications.”
For Kaasa, who has advised the WHO on its cancer work, the definition throws down a challenge to what he calls “mainstream oncology”.“Although palliative care, and palliative medicine as it’s also termed, has been around for a long time it is still not integrated properly into many cancer departments, which means patients can fall into gaps in their care,” he says. The problem, he adds, is that some health professionals – such as cancer doctors and nurses in hospitals – still see it as a specialism that is mainly about taking care of the dying and their families, and they worry that bringing it into the mainstream will mean pursuing futile oncological treatments.“Nurses, especially, may say that palliative care belongs in a nursing home or hospice, and if we work there we shouldn’t be part of acute medicine.”
Kaasa argues the opposite point of view. “Palliative care is important much earlier in the disease trajectory, especially as about 60% of cancer patients receive non-curative care. When you are giving chemo- and radiotherapy as part of life-prolonging treatment – where someone may live two to three years or more – they will have many symptoms and may often need to be supported at home.”There is so much new in oncology and in symptom control, says Kaasa, “Patients deserve to have palliative care specialists as part of the oncology team during their cancer journey. I strongly believe that oncology is better if the voice of palliative care is firmly integrated in the healthcare system.”
The WHO, he adds, has recently revised its definition of palliative care to include collaboration throughout the care pathway, and integration with oncology where appropriate. Those looking for a model of where that integration is taking place will find one at Trondheim, where Kaasa has also recently established the European Palliative Care Research Centre to drive the evidence base for his speciality.
There are a number of other compelling reasons for bringing palliative care into the mainstream, he notes. They include the best use of expensive treatments in metastatic disease – a huge issue for hard-pressed healthcare systems. Knowledge of metastatic disease itself is an underlying issue, given that it is often the poor relation of efforts put into the curative side of cancer treatment. Palliative care should also be pivotal in bringing together all the parts of healthcare systems and related professions that play a role in caring for cancer patients and their families, whether in the home or in primary care or acute settings. Everything from psycho-oncology to bereavement counselling and complementary therapies comes under the umbrella.
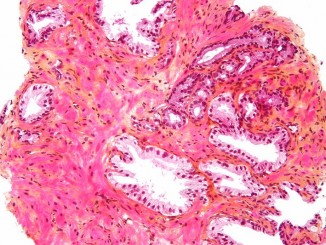
Among the general range of side-effects of progressive disease and treatments, two core symptoms stand out which can be extreme for many patients – pain and cachexia (muscle wasting).“In epidemiological studies on pain, about half of cancer patients are not sufficiently treated even when using opioids, and we know now that we need to start earlier when treating the many people with cachexia who have lost a lot of weight and muscle mass,” says Kaasa.
“We know now that we need to start earlier when treating the many people with cachexia”
As he explains, there is a great deal of research to be carried out on pain and cachexia, as well as on other aspects of palliative care. Such research includes a recent move to investigate biological mechanisms as well as clinical approaches that have been the mainstay. “The problem we have is that in pain, for example, the quality of evidence for management of people with cancer is very low– the studies are poor. There are too many small studies that are inconclusive – they don’t have the power we need.”
Fragmented research and small studies are common in cancer, he concedes, “but in palliative care it is even more challenging because patients are hard to reach and often very sick, and you need to design studies that can comply with an intervention or medication.”
Despite the lack of major studies, the last 10 years have seen a step up in focusing on palliative care and oncology in Europe. This is thanks in part to Kaasa’s success in putting the subject on the map in Trondheim when he moved there in 1993, as professor of palliative medicine at the Norwegian University of Science and Technology, which was one of the first such job titles in Europe at the time. He went on to establish a pain and palliative care research group that has carried out and coordinated many studies. “For example, we won an EU grant in the 6th framework programme in 2005 to co–ordinate the European Palliative Care Research Collaborative, under which we ran work packages on understanding and assessing pain and cachexia, and we also produced European guidelines on managing cachexia and depression.”
As always, the issue is the short-term nature of these programmes, and although there are other EU projects underway, Kaasa says that so far there isn’t anywhere near the critical mass of support for the wider collaboration and research networks he feels that palliative care needs.
While palliative medicine is by no means just about cancer, it is now such a major part of the speciality that the majority of his own researchers and clinicians in Trondheim are exclusively involved in oncology, as are other units with which they collaborate internationally in countries such as the UK and Canada. The European Association for Palliative Care (EAPC), for which Kaasa is a past president, has a strong oncology track and supported the establishment of the European Palliative Care Research Centre in Trondheim in 2009.
This cancer-only initiative is certainly one of the biggest steps forward recently, but Kaasa says the majority of its funding is from the Norwegian Cancer Society, and from his own hospital as well as the university. Without his vision for palliative care in oncology and the backing of Norway’s advocacy groups this centre would not be up and running, although it is attracting various grants from the EU and other sources, and of course enjoys the support of the EAPC and international colleagues.
Given his achievements so far, Kaasa is now aiming high at Trondheim – “I want to build a structure for integrated oncology and palliative care that will be a window for the world that will show what can be done,” he says. It’s an ambitious goal for what is a northern outpost in Europe, but as he says, he has already fought and won the battles to prove the need for integration locally, and with longstanding expertise in international networking there is every chance that he will ensure that Trondheim will be seen as the global model he envisions.
“I want to build a structure for integrated oncology and palliative care that will show the world what can be done”
Kaasa was a national cross-country skiing champion when at high school in Norway, and gained a great start for his early career when he landed a sports skiing scholarship at Denver University in the United States, where he was also able to model his own ‘pre-med’ course in anticipation of a return to Norway. Then in Oslo, he completed his medical training, taking in surgery, internal medicine and family practice. The latter was a career option until, unsure of what direction to take, he contacted Herman Høst, the ‘father ’of Norwegian oncology, and gained a short-term post at Oslo’s Radiumhospital.
“There I was challenged by a senior lecturer to look at lung cancer patients and the use of cisplatin in people with a short life expectancy, and I worked on a randomised trial between chemo- and radiotherapy, which was the basis of my PhD thesis. We were one of the first to actually ask people how they felt during their treatment – what we now call patient-reported outcomes – and our group was one of the movers in the development of the QLQ-C30 questionnaire at the EORTC for assessing the quality of life of cancer patients.”
It was the opportunity to do this kind of research that quickly convinced Kaasa that his career lay in oncology and not as a family doctor. He then gained his oncology board certification working on the spectrum of cancer issues at the Radiumhospital and, like oncologists in certain countries such as the UK and other Nordic countries, Kaasa is certified in both chemo- and radiotherapy, as a clinical oncologist. But his academic focus was on the non-curative side – and he duly completed a PhD on quality of life and survival.
“Although palliative care had been developed primarily in the UK back in the 1960s, thanks to the hospice movement, it was mainly outside of main stream healthcare. In hospital oncology it hasn’t really taken off until recently,” says Kaasa. “That’s because in the late 1980s we had a strong belief that we would see the sort of major improvements in cure rates that we had seen with testicular cancer and lymphoma, for example. When I was working on lung cancers we really thought we would cure them with high-dose chemotherapy and bone marrow transplants.”
Recent years have seen a repeat of this belief, he says, as the new targeted therapies have again pushed back palliative care to some extent, fuelled by the huge promotional activity of the pharmaceutical industry – although he adds that pharma was the first in offering support for quality of life studies when he was starting out. “Companies realised it was important to document subjective factors as well as response rate,” he says.
After establishing himself as a consultant oncologist in Oslo, the opening for the palliative medicine professorship in Trondheim came up. “In Norway we had been debating what we should do about palliative care and it was again the Norwegian Cancer Society that was instrumental in putting out a bid to set up a programme at one of our university hospitals. Trondheim won and I was asked to apply.”
Although Kaasa enjoyed the support of the hospital’s oncology department and the head of nursing, he still encountered most of the objections about actually integrating palliative care. “I won the battle by bringing in the academic side and starting a research programme, and putting a lot of energy into international collaboration and leadership. It’s hard for opponents to criticise solid research –especially as, after seven years or so, we were producing as much as 80%of the publications from the Cancer Clinic.”
Kaasa also argued from a clinical perspective that patients suffering, for instance, from pain with bone metastases needed to be treated with radiotherapy, and that to carry out academic medicine properly on such approaches palliative care had to be applied early in the journey rather than waiting for oncologists to deliver patients to palliative care professionals in another location.
From humble beginnings – when he started Kaasa had just one other doctor and two nurses –the palliative care team in Trondheim is now almost 30 strong, with molecular biologists and social scientists, more than 20 PhD students, a number of international researchers and visiting professorial placements, and various clinical and research input from other specialists in the university hospital, such as pain specialists.
Kaasa was asked to head the entire Cancer Clinic in 2010, and so is in the ideal position to oversee the integration he promotes. “And that’s what you would see is different here – palliative care doctors at our morning case meetings, which we hold every day. I don’t see patients myself now but I do become involved in particularly challenging cases.”
An early randomised study comparing specialist palliative care with care as usual, published in the Lancet, played a critical role in setting the agenda, says Kaasa. One major finding was that patients in the intervention group benefited from an integrated pathway by being able to stay longer at home. “An interesting spinoff was that the families reported better health even one year after the patient had died,” he says. Trondheim has now produced hundreds of studies related to palliative care, many of them in top-rated journals, according to Kaasa. Other studies have focused particularly on treatments, finding benefits for example in reducing the number of radiation fractions that need to be given to treat lung cancers and bone metastases, saving much trouble for patients and also costs.
“An interesting spinoff was that the families reported better health even one year after the patient had died”
Current research priorities for the field are revealed in a pan-European survey under an EU7th framework programme project called PRISMA, which shows that the top topics are pain, assessment tools, quality of death and last days of life, fatigue and cachexia, and family and carers. The main barriers are, inevitably, lack of funding, time, expertise and personnel.
Pain is still a major problem, says Kaasa. One reason he cites is that many patients are not diagnosed and followed-up appropriately. Another is that they do not receive effective treatments because they fall into gaps – a hospice physician may have no access to radiotherapy to treat bone metastases, while a radiotherapist may not know enough about opioids. “Optimal pain control needs a combined approach, including specialists at pain clinics. We have a close relationship with our pain clinic in Trondheim – but there can be little such collaboration between pain specialists and palliative care around Europe, as the pain clinics deal mainly with non-malignant conditions. We also have a growing population of cancer survivors who suffer non-malignant pain from side-effects later in life. We have to collaborate more for patients.”
One urgent need is to establish a consensus on pain assessment tools in palliative care and to update guidelines based on much stronger evidence. Kaasa points to some progress here: a recent special issue of Palliative Medicine (July 2011) published updated pain guidelines from the EAPC, the evidence base for a set of review articles, and there is now a much better platform on which to build cancer pain research.
Kaasa’s group is the leader of the European Pain Opioid Study (EPOS), which is a translational research project looking at the biological action of the drug. A major change in recent years, he notes, is a move to joining forces with basic scientists to research the biology of late-stage disease and effects, in addition to the patient-reported clinical studies.
“We have also been researching the genetic basis of pain to see if we could find a biomarker for pain response, but we had a negative result, which is still important to publish. We have been critical of the methodology often used in this type of research – those who go on ‘fishing trips’ for single nucleotide polymorphisms to find such biomarkers in clinical medicine, when there are so very few in use in oncology. But we have more encouraging signs for our work in cachexia.” (See box, below).
 One aspect of his field particularly annoys Kaasa, and that is terminology. As far as he is concerned, it is called ‘palliative care’ or ‘palliative medicine’ and should cover the vast majority of the advanced cancer journey. But he says confusion can be spread by the use of ‘end of life care’ and ‘supportive care’. “In some cancer centres this is often about competing for resources, with some focusing on what they call earlier symptom control in ‘supportive care’, while leaving others to do the ‘end of life’. Yes, if you have a large palliative care team you can have people focusing more on early symptoms, but really this is often about a resources battle and not integrated care, and of course again it is the patients who fall into the gaps.”
One aspect of his field particularly annoys Kaasa, and that is terminology. As far as he is concerned, it is called ‘palliative care’ or ‘palliative medicine’ and should cover the vast majority of the advanced cancer journey. But he says confusion can be spread by the use of ‘end of life care’ and ‘supportive care’. “In some cancer centres this is often about competing for resources, with some focusing on what they call earlier symptom control in ‘supportive care’, while leaving others to do the ‘end of life’. Yes, if you have a large palliative care team you can have people focusing more on early symptoms, but really this is often about a resources battle and not integrated care, and of course again it is the patients who fall into the gaps.”
A powerful way to get the message across about palliative care, he believes, is to have many more doctors gaining a palliative medicine qualification as an addition to their main work. “We now have a two-year course in the Nordic countries that we started in 2003, and it was officially endorsed, recently, for any doctor to study palliative medicine during their normal job, although they do have to take about six weeks out to attend the various modules, which are run at various locations in Scandinavia.” The Nordic Specialist Course in Palliative Medicine, as it’s called, is based on the British curriculum in palliative medicine, which is a standard for many countries.
There’s a big difference though between Britain and Norway when it comes to full-time palliative care practitioners, says Kaasa. “In Britain you can train from the start as a palliative medicine specialist, but here you need to have another speciality, such as oncology, first – all the palliative doctors in my unit are also oncologists.” In fact, one other issue he had to deal with on taking up his professorship at Trondheim was that his department was expected to handle conditions other than cancer, such as coronary heart disease and neurological illnesses.
“But to work in specialist palliative care you have to know the disease you are working with, in my view. After 10 years or so we stopped everything except oncology.” A cardiologist with a palliative medicine qualification is much better placed to work with heart patients, he says. “But outside the hospital a GP with palliative care knowledge can see everyone.”
“To work in specialist palliative care you have to know the disease you are working with”
An early success in clinical care in Trondheim was being allowed to involve multidisciplinary teams in seeing patients at home, and not just as in and out patients, which was a start in widening the care pathway. “There was no reimbursement system for visiting patients outside the hospital and so we went to the health authority and were granted a special arrangement – financial incentives can be very powerful in changing practice, I feel.”
Since then he has helped promote a palliative care strategy that works across all levels of health care, and which has been part of Norway’s cancer plan. Notable steps have been establishing service development units in each health region, encouraging more hospital directors to set up palliative care units, and making better provision for specialist beds in nursing homes. In 2004, a Norwegian standard for palliative care was published.
Kaasa has also made his mark in Norway in strategies for the wider healthcare system and the country’s cancer plan – among his many posts he is currently the national cancer director .He stresses how crucial it is to develop evidence-based guidelines in healthcare – guideline work has been among the more successful parts of Norway’s cancer plan. What many other countries lack, in his view, is the kind of palliative care model that Norway now has.
The EAPC, with partner organisations such as the International Association for Hospice and Palliative Care(IAHPC) and the Worldwide Palliative Care Alliance (WPCA), has set out a framework for development (the so-called Budapest commitments), which is an initiative aimed at national associations and includes defining standards of care. An EU 7th framework project, IMPACT (implementation of quality indicators in palliative care study), is looking at cancer and dementia care with work packages on organisation and implementation of care (see www.impactpalliativecare.eu).
These are good steps, says Kaasa, but Europe is some way from widespread quality-audited palliative care in a majority of oncology departments. He would like to see the EAPC gain funding to produce an oncology training curriculum, for palliative care to get a seat at the top table in ECCO, and for the subject to be addressed better at general cancer conferences, where it is often a side session that is not well attended. ESMO, the European Society for Medical Oncology, to which he belongs, could do much more on palliative care, he feels; in contrast, EONS, the nursing society “is much more supportive.” Next June, Trondheim is hosting EAPC’s 7th world research congress, which will be an ideal place to hear the issues first hand.
Again he mentions the value of politicians setting economic incentives to drive change, and Trondheim’s Cancer Clinic is an example of what can be achieved with integration – the number of beds has been cut from 68 to 36 following success in managing more cancer cases as outpatients – a caseload that is rising of course. “Metastatic disease incidence will increase 2% a year up to2020,” he says.
Not least of the issues is the cost of treatments in people with advanced disease, which Kaasa has also been advising the Norwegian authorities about. “We are seeing debates now about the cost–benefits of modern oncology even in the US – 10 years ago, the drug budget at our department in Trondheim was a tenth or so of what it is now.”He mentions a recent US study that randomised palliative care against mainstream oncology early in lung cancer. It found the intervention group lived longer and had fewer depressive symptoms, while the control group received more chemotherapy (NEJM 2010, 363:733–742).
The palliative care group lived longer, while the control group received more chemotherapy
Naturally, he may not be the most popular person with pharmaceutical companies, given his insistence for his team to use evidence-based approaches where possible even in advanced disease. “I’ve been in oncology a long time and I can see no major breakthroughs and just that growing metastatic burden.”He adds though that he is of course interested in promising drugs, and also in new uses, such as investigating how chemotherapy can be used to treat pain and other symptoms – an under-researched field.
There is still a pioneering air about palliative care in oncology given the major multidisciplinary research agenda still ahead, and indeed in the US a recent spate of articles in the mainstream media have just ‘discovered’ the speciality as an evidence based way to approach care for terminally ill patients, for whom futile treatment is common –countering the right-wing’s insistence that discussing end-of-life options will lead to rationing and bureaucratic ‘death panels’. Kaasa says Europe is ahead in models of palliative care, thanks to pioneers such as the UK’s Geoff Hanks, who was one of the founders of the EAPC, an advisor to the European Palliative Care Research Centre and a mentor when Kaasa was venturing into the field. “It was controversial when I started to focus on quality of life at the Radiumhospital, and I did push palliative care perhaps too strongly in the early years – but I think I was right,” he says.
Kaasa has four children and has remarried, to Anne Kari Knudsen, a pain researcher in his department. Skiing and fitness still play a big part in his routine.
“My aim now is to help establish a sustainable network of international centres conducting large scale research on palliative care in cancer, and in particular I want to gain new insights into pain and cachexia. I won’t stop pushing too for even better integration in Norway’s healthcare system. And I’ll stay here in Trondheim–the skiing’s better.”