With social media platforms, search algorithms and online research tools designed to let people upload, share, find and comment on information in real time, Sophie Fessl asks: why are we still reliant on a 350-year-old model for disseminating medical research?
“It is astonishing with how little reading a doctor can practice medicine,
but is not astonishing how badly he may do it.”– William Osler
Getting new evidence from clinical trial to the practising doctor requires two pieces to click: researchers need to publish their findings, and the doctor has to read them. Since the 17th century, the journal has been the means for this communication. Some processes, such as peer review, evolved to be crucial parts of journal publishing. With the internet revolutionising how we communicate, these ‘print-native’ processes are set to be overhauled by their ‘web-native’ counterparts – or have been already. “[…] the Web has irrevocably changed our information environment – it is no longer the habitat the journal evolved in,” publishing futurist Jason Priem argues in his opinion piece published in Nature (2013, 495:437–40). Whether or not the journal as we know it now survives in the digital age, the way a clinician seeks information from the literature may change dramatically in the future.
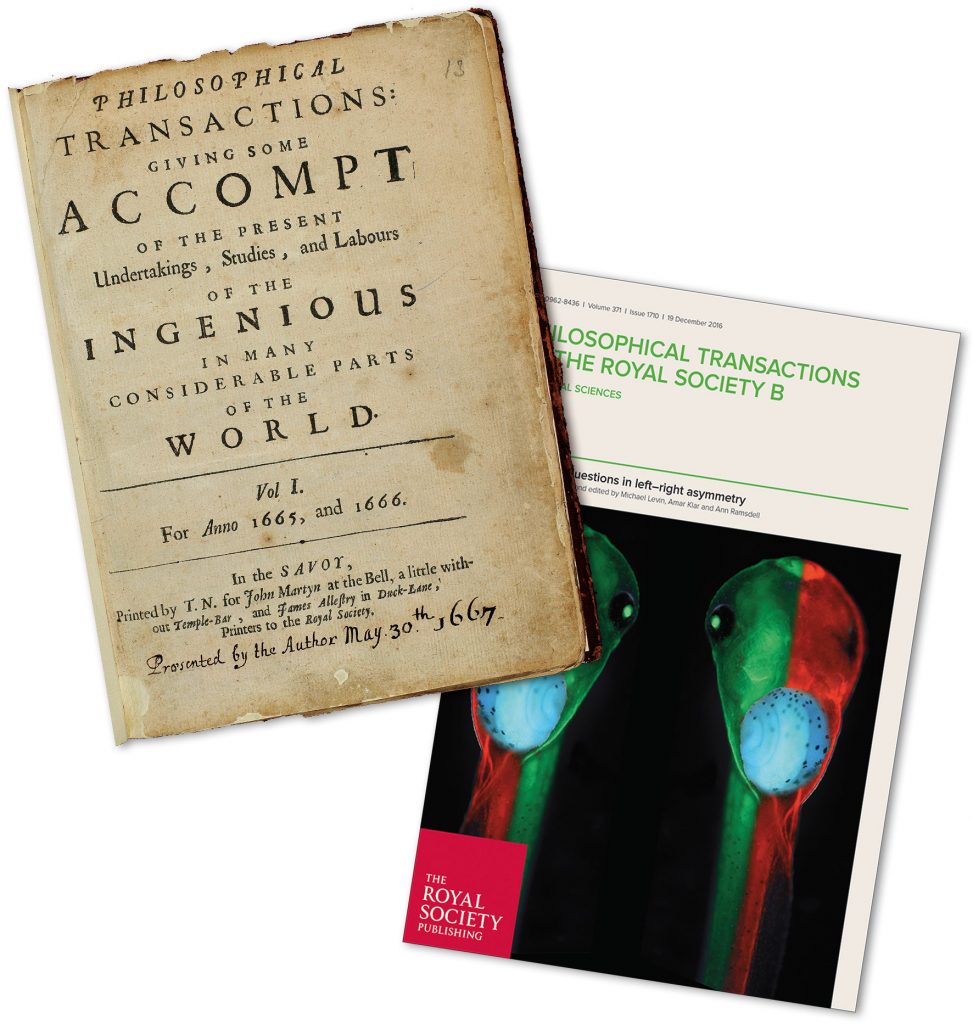
A 350-year history
In 1665, Henry Oldenburg founded the first English-language scientific journal, Philosophical Transactions of the Royal Society of London, to improve the dissemination of scientific knowledge. Before then, scholars shared their findings by sending letters to their networks of contacts. With the invention of the printing press, print materials could be mass produced and scientific knowledge spread widely. The first journals presaged some of the print-native elements of scientific journals: Philosophical Transactions were judged by Royal Society members, setting the framework for peer review, while Thomas Basset, editor of the first English medical journal Medicina Curiosa, saw his editorial responsibilities as guiding his readers to new information.
Medical journals unarguably proved a success; more than 25,000 biomedical journals are currently published worldwide. And yet, all is not well in the world of medical publishing. Peer review may have evolved since the 17th century, as a way to control the scientific quality of published papers, but in recent years it has increasingly come under fire. Richard Smith, former editor of the British Medical Journal, who spent some time studying the peer review system, reached the conclusion that it is “slow, expensive, ineffective, something of a lottery, prone to bias and abuse, and hopeless at spotting errors and fraud.” The benefits of peer review, he argued, have been much harder to establish (J R Soc Med 2006, 99:115–119).
Similar criticism has been levelled against the “impact factor”, a statistic that represents the mean number of citations to articles published in a given journal in the preceding two years. This metric was intended to function as an indication of the importance of a journal in its field, though interestingly it has also been found to predict for rate of article retractions due to fraud (PNAS 2012, 109:17028–33). A related problem is the way it has been widely
(mis)used as an indicator of the quality of work of academics who publish in them, including by research funders and appointment committees, which provides people with an incentive to fabricate or twist results to get published in the ‘best’ journals.
A few years ago the Wellcome Trust– the world’s largest medical research charity – announced it would no longer take into account journal impact factors when assessing the quality of research done by a grant applicant. Speaking to Cancer World, Robert Kiley, Head of Digital Services at the Wellcome Trust, said: “We need to move away from using the impact factor as a proxy for research assessment. It is a flawed metric… It is the intrinsic merit of the work, and not the title of the journal or the publisher with which an author’s work is published, that should be considered in making funding decisions.”
Focusing on readers’ needs
The greatest challenge for medical journals is how to present new findings in a way that doctors can best integrate them into their everyday practice. Twenty-five thousand biomedical journals is an impressive number, but with most doctors spending, by different measures, between one and three hours a week on professional reading, filtering what is most relevant has become a daunting task.
Marije Hamaker, a geriatric oncologist at the Diakonessenhuis in Utrecht, the Netherlands, who has helped develop an educational webcast on her speciality (e-eso.net, 30 June 2016), says
“I still believe that publishing in a journal has value in itself, as a means of spreading a particular message. But with so many journals around, I wonder how well read these journals really are and therefore how much that message is actually being received.”
Questions are being asked about whether the business model of journal publishing serves the interests of publishers better than those of academia, based as it is on authors freely contributing reports of research – frequently funded by charities or the taxpayer – which publishers then distribute back to the academic community at considerable profit to themselves.
While the internet and social media are unlikely to be a cure-all for the ills of academic publishing, they are already changing the shape of medical publishing: nearly 10% of journals are estimated to use social media, such as blogs, Twitter or Facebook pages, to allow commenting on articles. Lisa Hutchinson, Chief Editor of Nature Reviews Clinical Oncology, sees an opportunity in social media: “I think social media and the internet will greatly affect how doctors acquire information and gather evidence. To some extent, I don’t think this will negatively affect the ‘traditional’ formats in terms of how this guides daily practice. There are benefits and limitations to all aspects of medical publishing (whatever format), so this creates a more competitive environment, that will challenge business models currently and in the future.“
“I would define post-publication review as the process
whereby scientists and others decide
whether a piece of work matters or not”
For some publishing futurists, the internet can and should do more than just tinker with the existing journal model. It could revolutionise the way medical evidence spreads when print-native elements that make up a journal become disentangled. As Jason Priem argues, “the journal and article are being superseded by algorithms that filter, rate and disseminate scholarship as it happens,” (Nature 2013, 495:437–40). Rather than having more than 25,000 journals that each archive, rate and disseminate scholarship, a variety of interoperable, modular services could offer these traditional journal functions. These include certifications of peer review, web-based marketing, archiving, aggregated commentary and broad dissemination. Authors would be able to choose the services best suited for each purpose, adding certifications of peer review, significance, statistical review, altmetrics aggregators and more.
Opening access
While such a complete dissolution of the academic journal into a pick-and-choose self-publication model seems a long way off, the internet is already picking away at the subscription-only business model of publishing. Many journals have introduced delayed free access, but true open access publishing, with articles freely available upon publication, is changing the publishing landscape. Since 2013, the number of open access journals in the Directory of Open Access Journals has risen from 300 to 9,175. Last year, the Competitiveness Council – a gathering of EU ministers of science, innovation, trade and industry – called for all scientific papers to be freely available by 2020.
Open repositories, such as F1000Research, take the direction of open access journals a step further. They use the resources of the internet to make freely available the underlying data, analyses, and other publication formats such as posters. Last autumn, the Wellcome Trust launched Wellcome Open Research, a publishing initiative contracted out to F1000Research that, as Robert Kiley describes, “provides a platform in which our researchers can publish any research they think is worth sharing.” This platform, he adds, makes use of post-publication peer review, “and encourages the publication of all research outputs – case studies, datasets, protocols, null/negative studies as well as research articles.”
Kiley believes that by ensuring all research is available – and not hidden behind paywalls – and encouraging researchers to make available the data that underlie the research, open publishing may help doctors take evidence-based decisions.
Speeding up access
F1000Research and Wellcome Open Research are moving the point of peer review until after publication, so readers can access articles more quickly. Whether doctors should act on recently published information before reviews have come in will be left to their own judgement. A larger concern relates to the rigour and objectivity of the post-publication peer review, given that both systems leave it up to authors to invite people to review their papers. And while the system is intended to facilitate dynamic discussion of evidence, this is not always easy to achieve. PubMed Commons was launched in 2013, allowing users to comment on any of the 26 million research articles on PubMed. As of October 2016, only 4,523 have been commented on.
Former British Medical Journal editor Richard Smith argues that post-publication peer review is more about how a study is received: “I would define post-publication review as the process whereby scientists and others decide whether a piece of work matters or not… beginning to act on its conclusions, throwing it in the bin, and taking a thousand other actions that constitute the ‘market of ideas’” (BMJ 2010, 341:c3803).
Flagging up and filtering
Web-native processes are also likely to change how research impact is measured, adding new ways to find articles that others in a subfield deem noteworthy. New metrics of scholarly influence, ‘altmetrics’, track conversations generated by an article and include saves in reference managers, inclusion in public policy documents, or mentions on Twitter. These might also influence funding and hiring decisions, as researchers can begin to showcase their work’s diverse impacts in real time.
FOAM is a dynamic collection of resources and tools that include
blog posts, tweets, podcasts, videos, Google hangouts and more
When trying to find the evidence most relevant to them, publishing futurists foresee that doctors will come to rely on ‘personalised recommendation engines’, which provide a curated stream of the most important things to read. Moving from narrow, personally defined subfields to a wide subject area, the presented contents become increasingly filtered, with articles and other scholarly products, such as blog posts or videos that have been read/viewed, discussed, shared or cited by others in a field. With every interaction, such recommendation schemes become increasingly refined, like Google Search.
FOAM – The critical care model
Everyone can publish, market and share information on the internet. While journal articles and conferences were once the main conduit to presenting new research, the internet allows everyone to broadcast their ideas. In the field of emergency medicine and critical care, this gave rise to FOAM, Free Open Access Med(ical Ed)ucation. Michael Cadogan, who coined this term in 2012, describes the FOAM movement on his blog Life in the Fast Lane as “Medical education for anyone, anywhere, anytime”, and describes the material posted in the blog’s weekly review as “sophisticated, cutting edge learning resources that enable clinicians and students to update their knowledge and improve their understanding in a fun, motivating and time-efficient way.”
FOAM is a dynamic collection of resources and tools that include blog posts, tweets, podcasts, videos, Google hangouts and more. Social media are used to share and disseminate FOAM resources. On Twitter, for example, this is done by including a link to the resource and using the hashtag #FOAMed. A timeline of all tweets using that hashtag can be accessed by anyone, by using the search term ‘#FOAMed on Twitter’. Tweetdeck or similar apps also allow Twitter users to ‘follow’ hashtags, ensuring every post appears in their home Twitter timeline.
Some FOAM blogs, podcasts and websites directly provide educational resources, some compile conference talks, others highlight or review the literature. Rather than replacing journals, Michael Cadogan sees FOAM as “more akin to the editorials and commentary articles that appear in medical journals,” (Emerg Med Australas 2014, 26:76–83).
New hashtags have now emerged relating to different fields, eg #FOAMtox (toxicology), #FOAMped (paediatrics), and #FOAMim (internal medicine), whose subject matter sometimes extends beyond the emergency setting.
While there is as yet no #FOAMonc, several cancer ‘hashtag communities’ drive conversations between oncologists, researchers, and anyone affected by cancer. These communities centre around the different cancer types, which makes sense, and is probably an indication of the way these sorts of online cancer communities are likely to develop. The first community, #BCSM (breast cancer social media) started on July 4, 2011, with its first tweet chat. It has since been followed by others, such as for multiple myeloma (#MMSM), lung cancer (#LCSM), and neuroendocrine cancer (#neuroendocrinecancer).
While FOAM and #FOAMed conversations focus on promoting educational resources, the tweets tagged with the hashtags of cancer social media communities are conversations that touch on a range of topics, including advocacy and awareness, but also medical news and updates around relevant conferences. In tweetchats, participants usually discuss pre-set questions for which the patient perspective has a particular relevance, and tweets are archived and published on a website. Discussions of new evidence tends to peak when presented at major meetings, but new findings are regularly flagged up in tweets. While for FOAM, teaching tools and new evidence are collected in several websites, such as Life in the Fast Lane, such projects do not yet exist for resources in any field of oncology.
Several cancer ‘hashtag communities’ drive conversations
between oncologists, researchers, and anyone affected by cancer
Professional and educational organisations have certainly been making increasing use of social media to disseminate their own materials for many years. Andres Cervantes, who chairs the Education Committee of the European Society for Medical Oncology, cites the example of ESMO’s internet portal, OncologyPRO, a resource for members, “which not only focuses on educational material but also provides videos of ESMO congresses, symposia and educational meetings.” As congress attendance is decreasing, he adds, improving access to these resources is seen as a priority.
It has certainly proved invaluable as a way of disseminating ESMO’s clinical guidelines. “Every year, these guidelines are downloaded more than 1 million times, as all types of doctors need updates and the most recent data,” he says.
The European School of Oncology is also embracing the opportunities the internet offers for reaching more people at greater distances, by broadcasting publicly accessible fortnightly educational sessions as webcasts, in which participants anywhere in the world are able to pose questions and get responses in real time. These are archived at e-eso.net.
Moving towards a model where oncology professionals and the wider community see themselves less as recipients of education and more as participants in the process of flagging up, sharing and commenting on relevant material in real time is still rare in oncology communities. However, we can probably expect to see more hashtag communities emerge around different cancer types, and some of these may see the #FOAMed – Free Open Access Meducation – model as one to emulate.
Whether people are ready to dispense with the established pre-publication peer review process altogether, however, remains an open question. Geriatric oncology specialist Marije Hamaker has yet to be convinced. “I am not sure there is a good alternative [to academic journals], as I do believe that a process of peer review etc. is needed. The internet is full of information that has no scientific base, but is just someone’s opinion. I don’t know how else this process would work with sufficient quality control.”
FOAM pioneer Michael Cadogan, counters that “FOAM opinions and arguments live or die by being hammered on ‘the anvil of Truth’ that is free and open debate and discussion,” (Emerg Med Australas, 26:76–83). But it is the models being pioneered by the likes of F1000 Research and Wellcome Open Research that may point the way to the future for academic communications, based on open access, and immediate sharing of evidence with transparent review by peers, to “Enable(s) others to build upon new ideas right away, wherever and whoever they are.”
Time will tell whether their use of the internet will be as disruptive as Gutenberg’s printing press proved to be.


