Why do fewer people die of cancer in my neighbourhood than on the other side of town? Steve Buist of the Hamilton Spectator asked this question of his home city in southern Ontario, and used a variety of local data and sources to find answers. The story he told, using interactive maps and personal stories, won him the Best Cancer Reporter Award 2014. We reprint an edited extract.
 Ask any cancer survivor and they can recall in vivid detail the day they heard the dreaded words “You’ve got cancer.”
Ask any cancer survivor and they can recall in vivid detail the day they heard the dreaded words “You’ve got cancer.”
It’s been 42 years since US president Richard Nixon launched the so-called war on cancer, and yet four decades later, with a cure as elusive as ever, cancer still scares us to the core. Is it the perverse lottery aspect of getting cancer that scares us most? The idea that you can be living your life and then – without warning, without a sign – a switch gets flipped somewhere inside your body and this ticking time bomb is lit?
Even when the link between cause and effect is clear and irrefutable, there’s still a randomness to getting cancer. We all know there’s a strong connection between smoking and cancer yet three out of four regular smokers will still somehow manage to escape lung cancer. Or is it cancer’s lethality that scares us most? We know there’s a randomness associated with that, too. Some people beat it, others die from it.
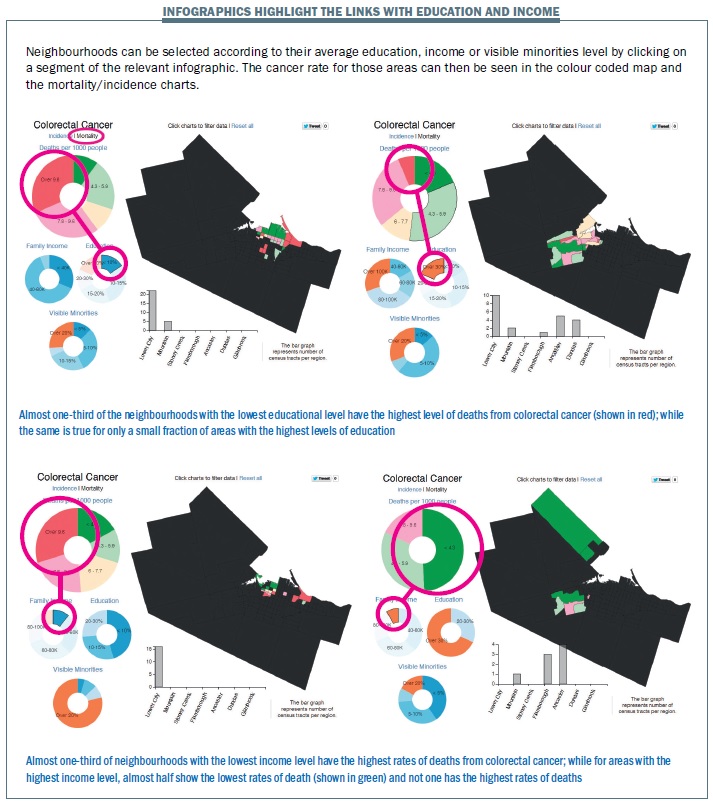
But what if dying from cancer isn’t as random as we believe? What if your ability to survive cancer has something to do with the size of your paycheque or the amount of education you’ve had?
That’s what the findings of The Spectator’s exhaustive new cancer investigation strongly suggest. Ten years of data broken down to the neighbourhood level show that poorer people in Hamilton, on average, are dying of cancer at significantly higher rates than richer people. One neighbourhood in the inner city core, for example, has a cancer death rate that’s four times higher than a neighbourhood in Ancaster, the city’s wealthiest suburb.
The question is why? Why are poorer people dying of cancer more frequently than richer people? The reasons are enough to shake one’s faith in this country’s beloved universal health care system, long presumed to be the great equalizer that bridges the gap between the haves and the have-nots.
Why are poorer people dying of cancer more frequently than richer people?
Our comprehensive analysis shows significant disparities when it comes to access and utilization of basic health services such as cancer screening programs and family physicians.
What’s disturbing is that those disparities often play out along social and economic lines. When it comes to cancer screening programs for breast, cervical and colorectal cancer, people in Hamilton’s poorer inner-city neighbourhoods are being screened at much lower rates than people in the richer suburbs of Ancaster, Flamborough, Dundas, Glanbrook and Stoney Creek. In some cases, the screening rates are nearly three times greater in the wealthiest neighbourhoods compared to the poorest ones.
An exclusive Spectator survey also shows that people in the inner-city core are three times more likely not to have a family physician and twice as likely to use walk-in clinics as their main source of health care than people in the western suburbs of Ancaster, Dundas and Flamborough. The investigation also shows that frighteningly high rates of smoking in Hamilton’s inner city play a major role in the high cancer death rates that affect the city’s poor.
Let’s start with cancer screening programs and the example of one specific inner-city neighbourhood, the chunk of downtown Hamilton between James, King, Wellington and Cannon streets. Nearly half of all adults and almost 70 per cent of children there lived in poverty, according to the 2006 census – the highest rates of poverty in the entire city.
That area also happens to have the highest cancer mortality rate in Hamilton, four times higher than an Ancaster neighbourhood that has the lowest death rate.
Now look at the cancer screening rates for that same inner-city neighbourhood. Just 29 per cent of eligible women were screened for breast cancer in 2009, the lowest proportion in Hamilton. By comparison, the highest rate was one Glanbrook neighbourhood where 75 per cent of eligible women were screened.
Just 21 per cent of eligible men were screened for colorectal cancer, and again, that was Hamilton’s lowest rate. In the best neighbourhood – again in Glanbrook – the rate was 55 per cent. When it comes to screening for cervical cancer, it’s the same story. Only 34 per cent of eligible women were screened, compared to 78 per cent in one Flamborough neighbourhood.
Maybe it’s just a coincidence that the neighbourhood with the highest rate of poverty and highest rate of cancer deaths also has the worst rates of screening for three common types of cancer. Or maybe it’s not a coincidence at all.
Pull the camera back a little further and the same picture keeps coming into focus.
The Spectator’s investigation shows the cancer death rate in the inner-city between Queen Street and Parkdale Avenue from Main Street to the waterfront was 90 per cent higher than the death rate in Ancaster, the city’s wealthiest suburb. At the same time, the rates of cancer screening across the board in the inner-city are one-third lower than the rates in Ancaster.
In the core, 47 per cent of eligible women were screened for cervical cancer in 2009. In Ancaster, the rate was 68 per cent. For colorectal cancer screening, the rate in the core was 33 per cent of eligible men and 40 per cent of eligible women. In Ancaster, the rates were 48 and 54 per cent, respectively.
In every case, it’s the same story. Screening rates improve as you move from areas of low income to areas of higher income. When it comes to breast cancer screening, 45 per cent of eligible women in the inner city were screened. In Ancaster, the rate was 67 per cent. If you ranked amalgamated Hamilton’s 135 neighbourhoods from top to bottom for breast cancer screening, the bottom 32 neighbourhoods with the lowest rates are all found in the lower part of the former City of Hamilton.
Screening rates improve as you move from areas of low income to areas of higher income
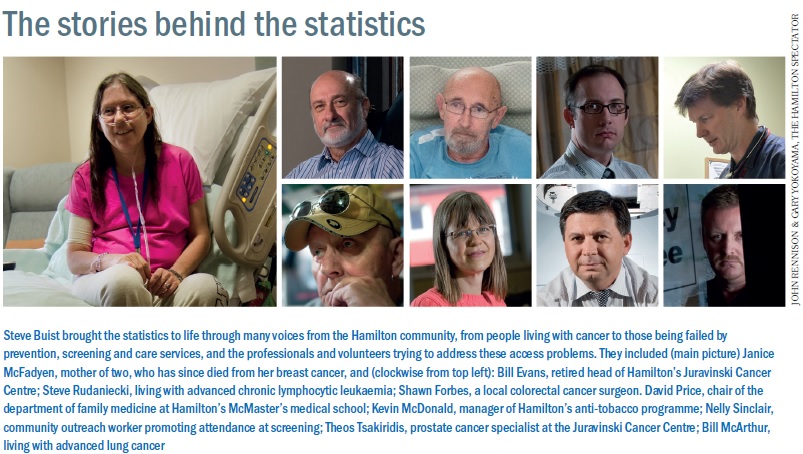
Ontario’s target for breast cancer screening is 70 per cent of women ages 50 and older. Only three of Hamilton’s 135 neighbourhoods have attained that level, according to the data provided to The Spectator by Cancer Care Ontario. It’s taken over 15 years to even get that close to the target, said Dr Bill Evans, recently retired head of the Juravinski Cancer Centre. “Why is that?” Evans asks, then answers. “Well, we keep doing the same thing over and over again. “We promote it in Chatelaine magazine,” he said, speaking about breast cancer screening programs. “Guess what? The folks down in north Hamilton aren’t reading Chatelaine.”
The disparities in screening rates are another sign of the strong connection between health outcomes and social factors, Evans noted. “It goes back to an awareness of what are the healthy behaviours, including going for screening, having your Pap tests, having your colorectal screening and breast screening,” Evans said. “All of those things are partly determined by your level of knowledge and understanding. “If you’re in less well-off circumstances, you might not know those things or you might not know how to find them or you can’t afford to get to them,” he added.
It’s important to note screening programs don’t change the incidence of cancer. But they should ultimately improve the outcomes for those who are screened and found to have cancer. “As you keep going in the breast screening program, you expect that you’re going to pick up smaller and smaller cancers,” said Carol Rand, director of systemic treatment and regional cancer programs at Juravinski. “That’s the definition of being a good screening program. “You’re not a good screening program if you’re just picking up great big cancers,” she said. “People are already well advanced at that point.”
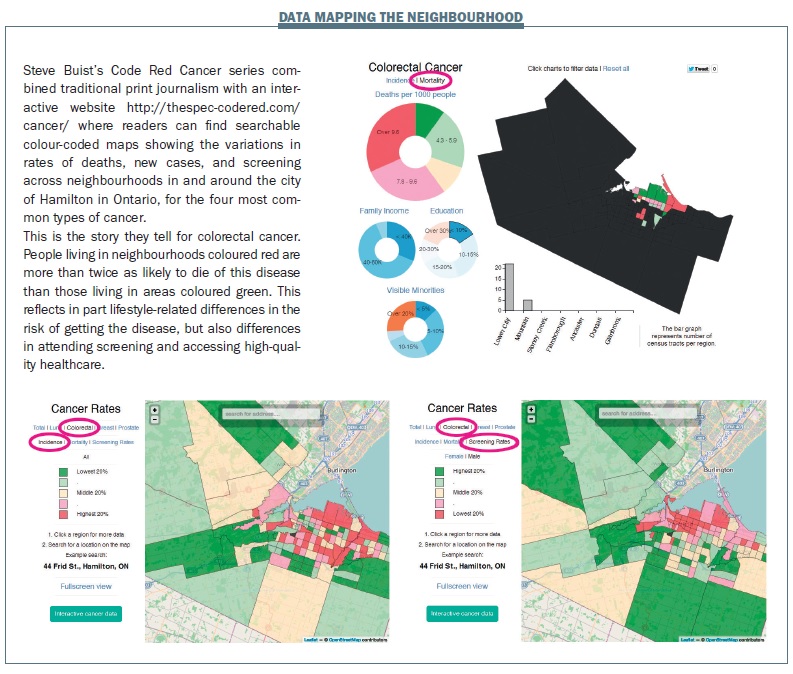 Shawn Forbes is a colorectal surgeon specializing in cancer at the Juravinski centre. Originally from Thunder Bay, Forbes came to Hamilton to attend McMaster’s medical school then decided to stick around. He has no shortage of work here, that’s for sure. Between 2000 and 2009, about 3,250 people in Hamilton were diagnosed with colorectal cancer, and more than 1,400 people died of the disease. The Spectator’s landmark cancer analysis shows there’s a notable income gradient in colorectal cancer mortality rates across Hamilton. The death rate from colorectal cancer in Hamilton’s east end between Parkdale Avenue and the Stoney Creek border was about 80 per cent higher than the colorectal death rate in Flamborough. The numbers are sobering, Forbes said.
Shawn Forbes is a colorectal surgeon specializing in cancer at the Juravinski centre. Originally from Thunder Bay, Forbes came to Hamilton to attend McMaster’s medical school then decided to stick around. He has no shortage of work here, that’s for sure. Between 2000 and 2009, about 3,250 people in Hamilton were diagnosed with colorectal cancer, and more than 1,400 people died of the disease. The Spectator’s landmark cancer analysis shows there’s a notable income gradient in colorectal cancer mortality rates across Hamilton. The death rate from colorectal cancer in Hamilton’s east end between Parkdale Avenue and the Stoney Creek border was about 80 per cent higher than the colorectal death rate in Flamborough. The numbers are sobering, Forbes said.
“The way our health care system is set up is a universal system and everybody should have equal access,” said Forbes. “But these numbers would suggest otherwise. Unfortunately, there is no one individual marker or test or indicator of socioeconomic status that encompasses the entire problem,” he added. “If only there was a single marker that could say, OK, this is a population that is at risk.”
Screening rates for colorectal cancer lag behind those for breast and cervical cancer, and again, there’s a significant difference across income levels. There’s also a notable gender difference – women take advantage of colorectal cancer screening more than men. In one inner-city neighbourhood, just one in five eligible men were screened in 2009.
The good news is that colorectal screening rates through the use of a fecal occult blood test rose dramatically in the amalgamated city of Hamilton between 2005 and 2011. The bad news is that even with the increase, just 30 per cent of Hamilton’s eligible population completed the test.
It’s important, Forbes said, to remember the fundamental reasons for cancer screening programs such as FOBTs and colonoscopies. “We screen because a disease is common,” he said. In the case of colorectal cancer, it’s the third most common type of cancer in men and women in Hamilton. But we also screen for colon cancer and a number of other cancers because we can modify the outcome and that’s the big deal,” he said. “If screening didn’t affect the outcome, then we wouldn’t screen. But we know that if we catch colon cancer early, we can modify the outcome and improve survival rates.”
When colorectal cancer is diagnosed at stage I, the five-year survival rate is 93 per cent, according to the American Cancer Society. But stage IV colorectal cancer? The five-year survival rate is less than 10 per cent. “We know that stage is the biggest predictor of mortality,” said Forbes. One of the questions he’s been helping research recently is whether or not there are differences in tumour stages based on a patient’s socioeconomic status. “If there are more advanced-stage tumours coming out of the core or those with lower socioeconomic status, then it has something to do with diagnosis,” said Forbes. “Are these people not getting screened as aggressively as people of greater wealth?”
One of the barriers to colorectal screening is the stigma that comes attached with the disease. For some people, it’s a squeamish and uncomfortable topic they’d rather avoid. “Even when they come to me – and this is all I do, this all I talk about – you can see they’re embarrassed,” said Forbes. “There’s nothing embarrassing about it. This is your life, this is your health we’re talking about.
“We’re here to help,” he added. “There’s a reason we’re doing this.”
 Nelly Sinclair is a community outreach worker with the CASTLE project. Funded by the Public Health Agency of Canada, the goal of CASTLE – Creating Access to Screening and Training in the Living Environment – is to increase the woefully low cancer screening rates in three inner-city neighbourhoods.
Nelly Sinclair is a community outreach worker with the CASTLE project. Funded by the Public Health Agency of Canada, the goal of CASTLE – Creating Access to Screening and Training in the Living Environment – is to increase the woefully low cancer screening rates in three inner-city neighbourhoods.
Since the start of the year, Sinclair has been to more church basement dinners, retirement homes, afternoon teas, group homes, seniors’ aquatic programs and community meetings than she can count in the McQuesten, South Sherman and Crown Point neighbourhoods. “It’s got to be the best job in the world because building relationships is a lot more fun than working,” said Sinclair.
Gently, patiently, persistently, she’s trying to persuade people to get screened for breast, cervical and colorectal cancer. At times, it seems like a person-by-person campaign. “They’ve got the majority of the people who are easy to do,” said Sinclair, who is 46 years old. “I’m there to try to find the ones that aren’t easy and to make change with them.”
Gently, patiently and persistently, she is trying to persuade people to get screened for cancer
In some of the neighbourhoods she’s responsible for, less than 30 per cent of eligible men had been screened for colorectal cancer and fewer than 40 per cent of eligible women had been screened for breast cancer prior to the start of the CASTLE project. “People don’t change just because you tell them they should,” she added. “There are many good reasons why people are not doing cancer screening so my job is to find out what those reasons are and to get these people to the point where they’re actually going to do the screening.”
A pastor’s wife, Sinclair, her husband and their four children moved to Hamilton two years ago from Alberta. She’s not a health care professional by training – in fact, she was hired precisely because she wasn’t one. For the people she’s trying to reach, health care professionals can sometimes seem scary.
“When I talk with somebody, I start with where they’re at and what their story is and where do we go from there,” Sinclair explained. “The conversation’s not finished if we’re not talking about cancer. If they don’t want to talk about cancer screening today, I’ll be back next week,” she said. “Whereas a health professional is providing a service, they let you know what the service is and then you come when you’re ready. I go to where they are when they’re not ready and try to work at that.”
She tells the story of one man at a group residence who she convinced to take the fecal occult blood test after many weeks of effort. Along the way, she also had to help him navigate his way to finding a new doctor located closer to where he lives. “When I first talked to him, there was no way under the sun he was ever going to put his poop in the mail and he told me so in no uncertain terms,” she said with a laugh. “So it’s a process.”
His case highlights some of the barriers she’s found along the way – attitudes to screening, access to a health care professional, transportation. She’s also seen the barriers placed by mental health issues when it comes to screening. Sinclair recalled the time she was in a convenience store and ran into a man she’d been trying to convince to go for colorectal cancer screening. “I asked him how he was doing and he said ‘I had a really bad weekend,’” Sinclair said. “‘I was in the hospital, I tried to commit suicide.’
“You learn that sometimes you have to back off with some people because their mental health issues flare up,” she added. “It’s real life, it takes priority.”





Leave a Reply