Patients who have run out of options don’t have time to wait for lengthy trials. But they also need treatments that offer proven benefit, and not just hope. Peter McIntyre asks whether we can speed up the learning process without sacrificing certainty.
Shortly before Robert Califf was appointed head of the US Food and Drug Administration in February 2016, he told a seminar in Washington that clinical trials were regarded as “too slow, too expensive, not reliable, and not designed to answer the important questions”. His priorities include streamlining clinical trials to make better use of real-world data in “a learning healthcare system”.
The views of the man who heads the US regulatory body reflect widely expressed opinions in Europe among researchers, patients and industry. Some suggest that the days of the gold standard randomised controlled trial (RCT) are numbered, arguing that they take too long to answer a single question, and condemn too many patients to stay on a treatment arm that is not working for them in order to generate the required statistical significance.
“You would not buy
a mobile phone today
based on a review
of phones in 2005”
Iain Galloway
There is also an increasing demand for ‘real world data’ from high-quality registries to supplement or even replace traditional clinical trials, to demonstrate the effectiveness of promising new treatments in everyday practice, and to define the sub-groups who best benefit from molecular targeted therapies and immunotherapy. There are concerns, however, that abandoning RCTs could open patients up to untested treatments that will turn out to have limited impact on overall survival.
Wrong questions, too slow
The weaknesses of the traditional approach are felt most in rare cancers (collectively 22% of cancers in Europe) and in cancers with limited treatment options and low overall survival. A consensus paper from Rare Cancers Europe in 2014 called for new approaches to collect and analyse evidence, using adaptive trial designs that feed performance data back during the trial, allowing patients to switch treatments. The availability of electronic patient records and patient-reported outcomes, it argued, make it possible to use retrospective cases as surrogate control arms.
Iain Galloway runs the Ocular section of the Melanoma Patient Network Europe, and is strongly campaigning for better trials. Ocular melanoma is a very rare cancer and about half of patients develop liver metastases, with a very poor prognosis. Galloway, who has a full-time job and a family, has himself had a large part of his liver removed, and is now on pembrolizumab. Though currently well, he is looking ahead to next steps should his disease progress, and he feels too little effort is being made to investigate new options for people in his position.
Galloway has written to the NHS England Specialised Services Clinical Reference Group complaining of the treatment options offered in England to the 200 or so people who develop metastatic ocular melanoma every year, saying many are “sent to die on useless treatments such as dacarbazine,” which has no long-term clinical benefit.
Some patients are so desperate, he says, that they seek places on skin melanoma trials of BRAF inhibitors, even though mutations in the BRAF gene are very rare in ocular melanoma. “We are subjected to ineffective trials that are not going to benefit us. It is little more than intellectual masturbation,” he says.
“We can’t afford to wait
five or 10 years while one
medicine wends its way
through the lengthy traditional
trial process” Kathy Oliver
At the same time, he adds, patients may be missing out on treatments that really could help them because of what he sees as the ‘outmoded’ way health technology agencies conduct their analyses. He cites, as an example, a chemosaturation approach to treating the sort of diffuse liver metastases typically associated with ocular melanoma. This involves isolating the liver and saturating it with high concentrations of an alkylating agent (melphalan), which is then filtered from the blood before it flows back to the heart.
In May 2014, NICE, the health technology assessment (HTA) agency for England and Wales, found limited evidence of effectiveness, with a significant incidence of serious adverse effects. In July 2016, NHS England concluded that “there is not sufficient evidence” for chemosaturation to be routinely commissioned, on the grounds that that the studies they looked at were small and lacked control groups and none were of high enough quality to draw firm conclusions on safety.
Galloway acknowledges that the filtering of the toxic treatment was inadequate in early trials, but says that adaptations have been made on the basis of early experiences, and that NICE and the NHS are failing to keep up. “You would not buy a mobile phone today based on a review of phones in 2005, and these cancer treatments are changing at about the same speed,” he says.
A study of 20 consecutive patients published as a poster presentation at ASCO 2015 (JCO 33, 2015, suppl; abstr e20000) recorded no treatment-related mortality, with only one grade 4 event and five grade 3 events. Thirteen patients (65%) showed a partial response in the liver and two patients (10%) showed a complete response. At the time of publication, 55% (n=11) had survived for one year, and 15% (n=3) for more than two years – compared to a one-year survival rate of 15–20% without the treatment. “The research team concluded that chemosaturation can provide significant benefits in a carefully selected group of patients as part of a multidisciplinary approach.”
As is often the case with very rare cancers, the metastatic ocular melanoma patient community is well networked, and Galloway says the results presented at ASCO reflect the positive experiences of many who were part of that study, which was conducted at the Southampton University Hospital in the UK.
“We don’t learn systematically,
and that is for me
a terrible waste”
Bettina Ryll
He wrote to the group that reviewed the treatment for the NHS, saying “It is evident that those who benefit from chemosaturation have a very high quality of life and suffer very few of the side effects noted in your research. It appears that your research is woefully and unacceptably outmoded. Adverse effects reporting and treatment morbidities are now very considerably lower than those stated in your statistics.”
Kathy Oliver, co-director of the International Brain Tumour Alliance agrees that patients with aggressive cancers need rapid access to effective treatments, and don’t have time to wait for a succession of lengthy RCTs.
“The median survival for a patient with glioblastoma [GBM – a highly aggressive brain tumour] – is about 14.6 months, so we urgently need new drugs to be developed quickly. We can’t afford to wait five or ten years while one medicine wends its way through the lengthy traditional trial process. “Our patient population is desperate, and one of the ways they can possibly have a chance of surviving a little bit longer is to try innovative approaches.”
These approaches are at the heart of the GBM AGILE trial that will start recruiting patients in the USA, Australia, China and Europe in the autumn, under a master protocol agreed with the FDA. Initial drug treatments will be based on genetic markers found in each patient and the trial will be guided by Bayesian statistical approaches.
Treatments will be adapted as centres learn what works and what does not, so similar patients (as determined by subtypes and enrichment biomarkers) will have a higher probability of being assigned to something that might benefit them, and will be less likely to be randomised to agents that perform poorly in their subtype.
Anna Barker, director of the GBM AGILE trial, is a former deputy director of the National Cancer Institute and was one of the founders of The Cancer Genome Atlas project (TCGA).
“The Cancer Genome Atlas has created literally thousands of investigations about the pathways involved in this disease, so we have a pretty good sense of the genes that are perturbed in these pathways and we know certain biomarkers are of potential significance.
“Almost any drug that has not yet been tested in GBM could be a candidate because we don’t know what is going to work in this disease.” Barker says that they may also retest some drugs that were deemed to have failed in the past. “There are all kinds of reasons why these drugs have failed, and frankly there may be drugs out there already tested in GBM but just not tested very well.”
She hopes the evidence generated will enable them to pick strong potential ‘winners’, good enough to show their value in short, small phase III trials.
It is not only rare cancers where patients believe trials are failing them. Many people with cutaneous melanoma – diagnosed in more than 100,000 people in Europe each year – feel the same way.
Before the arrival of new immunotherapies, the median survival time for patients with stage IV metastatic melanoma was less than a year. Bettina Ryll watched her husband die from the disease at a time when new treatments were just within reach, and founded Melanoma Patient Network Europe to campaign for better treatments.
“I don’t think you can
defend yourself by saying
that the patient wants it.
Hope sells just about anything”
Lex Eggermont
She says that the design of clinical trials needs to keep pace with molecular and medical advances to ensure rapid learning. Patients in desperate situations need early access to promising drugs, combined with systematic data capture about safety and efficacy.
“We are running trial designs invented 50 years ago to deal with a situation that has fundamentally changed. Our people were dying in six to nine months, so any uncertainty should be compared to that timeframe. Running one RCT – which takes time to plan and prepare and start and see it published – before starting the next one, is a very inefficient way to generate evidence.”
Opportunities are still being missed, she says, citing as an example an early access programme for a PD-1 antibody which collected data on safety, but not on efficacy. “We don’t learn systematically, and that is for me a terrible waste.”
Don’t sacrifice reliability
Amidst all the calls for change however, some of Europe’s leading cancer specialists are warning that the security and confidence generated by RCTs must not be put at risk.
Lex Eggermont, director general of the Gustave Roussy Institute, Paris, accepts that special measures are required when breakthrough therapies appear for rare cancers, but says that the level of evidence must remain high before introducing expensive new treatments for large groups of patients where there is already treatment available.
“What is not well understood by the public is that RCTs protect you against overtreatment and what I would call ‘religion’ rather than ‘science’.
“It is very risky to drop the mechanism by which we compare our standard therapy to new treatment and go through a rigorous evaluation of whether the benefits are truly what we think they are bringing.
“We have been wrong so often in the past. Randomised controlled trials demonstrated that the benefit was totally marginal and in no way justified the costs and the associated toxicity. If we make conclusions without randomised controlled trials, it would mean that we have not learnt anything from our past experience and declare that our understanding is so much more profound. This is a very dangerous path.”
The fact that the new therapies hold so much promise makes RCTs even more important, he says. “We need to keep our heads cool to ensure we are not going to prescribe all sorts of stuff that has marginal activity and actually would block patients from getting access in a couple of years from now.”
Eggermont is concerned that there are few reliable biomarkers for testing who benefits from new immunotherapies, and doubts whether governments and insurance systems will pay €160,000 a year for a new treatment unless they are confident it will show results.
He points to the huge off-label demand in the US for checkpoint immune blockers for indications where there is little or no data. “People are selling their houses and sacrificing the college funds of their kids, and if the kids are already independent, they feel forced to sell their house as well, and this is all based upon nothing. I don’t think you can defend yourself by saying that the patient wants it. Hope sells just about anything.”
Fatima Cardoso, Director of the Breast Unit at the Champalimaud Cancer Clinical Centre in Lisbon, also advises caution. Novel trials help to form treatment hypotheses, she says, but do not provide final evidence. “As far as I am concerned, at the moment, I don’t think we can move away from these phase III trials.”
“One reason for slow progress in metastatic cancer
has been the acceptance of inadequate endpoints
such as progression- free survival” Fatima Cardoso
She is concerned that pertuzumab (Perjeta) has been approved in Europe as a neoadjuvant treatment for early breast cancer on the basis of pathological complete response in a phase II trial – a finding that does not always translate into best survival or fewer relapses.
Such early approval is acceptable in areas of unmet need, she says, but not where there are already good treatments. “For pancreatic cancer I would be totally OK with providing temporary or conditional approval pending phase III results. For early breast cancer it is quite a stretch to say this is also unmet need.”
Cardoso argues that one reason for slow progress in metastatic cancer has been the acceptance of inadequate endpoints such as progression-free survival. Progression-free survival for the metastatic patient does not make a difference to how long you survive, she explains. “Basically it means that you are going to die the same day, but you will die with or without progression of your disease for a few more months. That is only meaningful if the patient has a lot of unpleasant symptoms from their disease, in which case it is very important that you control the disease. In breast cancer most of the time progression does not lead to significant symptoms.
“I am always fighting for our end point to be survival: only drugs that really increase survival should be given priority.”
Real world learning
One solution increasingly talked about is to do a lot more learning outside of trials, within registries, where data are systematically collected on patients treated in a real world setting. This has the advantage of showing how new treatments perform in their intended patient population, as opposed to the selected group who make it into trials.
The European Cancer Drug Development Forum held a workshop in July on the use of real world data to optimise oncology drug development and access. The workshop – attended by regulators, clinicians, HTA/payers, and policy makers – focused on how to generate evidence on efficacy and safety in the real world setting in a way that would also inform reimbursement decisions.
Richard Bergström, Director General of the European Federation of Pharmaceutical Industries and Associations (EFPIA), strongly supports such an approach. He points out that people were sceptical about the difference that drugs like Herceptin would make, even after successful clinical trials. Now many are used in an adjuvant setting, with dramatic results. “You have real population outcome data and you see stark differences. That is very difficult to disagree with. That suggests that we should capture data in real time in real lives. We should not have to wait 10–12 years for some academic to come and do this.”
“We need data capture for every patient
going forward in real time,
so we get real world evaluation
both for effectiveness and for value”
Richard Bergström
He has a vision of ‘super centres’ for cancer that are able to offer all promising new treatments and capture data on efficacy and safety in highly computerised registries. Patients can be stratified according to prior disease, age, sex and other variables, and randomised to different new treatments, based on advanced molecular diagnostics. This, says Bergström, would lead to more rapid learning of how best to use new therapies and in which patients, and would speed up access to new treatments.
“We need data capture for every patient going forward in real time, so we get real world evaluation both for effectiveness and for value. You can then do payment by results for one-year, two-year or three-year survival.”
Generating this sort of data would require much better sharing of data through well organised registries.
It would also require a change of culture in the prestige and attention given to reports of real world data. Martine Piccart, Head of the Department of Medicine at the Institut Jules Bordet, points out that at international conferences clinical trial reports are usually delivered from the platform, while real world results are not. “If you submit a study of 1,000 patients who have been treated with new drug x after registration in the real world, most of the time you will end up in a poster presentation and that is a pity.”
Change is coming
The growing influence of cancer patient advocacy means that change will happen one way or another.
Kathy Oliver from the International Brain Tumour Alliance accepts that it is tough for clinicians to move away from the randomised controlled trial as the gold standard for evidence. However, her son Colin died from a brain tumour in 2011 at the age of 32 and she says that patients with rare and intractable cancers do not have time to waste. “Progress in brain tumour treatments is far too slow. We need to really get a move on here, challenge the status quo and think outside the box.”
Iain Galloway’s group is developing criteria for a traffic lights system for ocular cancer, with amber warning lights for melanoma trials that test promising new treatments against something old-fashioned and ineffectual. “We have now some drugs with amazing efficacy and they cannot be trialled against old chemotherapy.”
Bettina Ryll warns that better-informed patients will no longer accept being on ineffective treatment arms. “In the past we wrapped it up as good research and sold it to patients as ‘heroes’ on trials. People are less and less willing to put up with it. They will vote with their feet and empty the trial.”
Testing by pathway
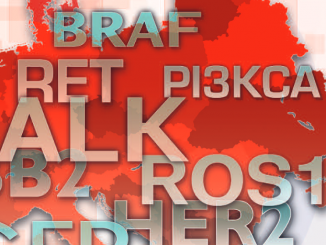
One approach to developing new treatments is to target molecular pathways across several tumour types, rather than focusing on a single histological site. Denis Lacombe and colleagues at the European Organisation for the Research and Treatment of Cancer explored “histology agnostic cancer clinical trials” in a 2014 paper, in which they argued that drug development one cancer site at a time can be “inefficient, time-consuming and expensive” (Mol Oncol 2014, 8:1057–63).
Channelling patients to trials on the basis of genetic markers is what lies behind EORTC’s SPECTA programme, and it is also the basis for the US-based NCI-MATCH trial.
NCI–MATCH focuses on patients
who are not responding to standard therapyNCI-MATCH focuses on patients who have solid tumours or lymphomas that are not responding to standard therapy. Through DNA sequencing, patients will be evaluated for inclusion on one of 24 treatment arms trialling drugs approved for another cancer indication or under trial. They include inhibitors that target EGFR, HER2, MET, ALK, BRAF, FGFR and other markers.
Overall 5,000 patients will be screened for 4,000 genetic variations across 143 genes. Those who are put onto treatment arms will continue for as long as the tumour shrinks or remains stable. If treatment fails they may be considered for a second arm of the trial. The aim is that at least 25% of patients will have rare cancers. Drugs that produce promising results may be incorporated into larger future studies.
While there is huge interest in this pioneering trial, NCI-MATCH also demonstrates the limitations of this approach. Only 9% of the first 500 patients assessed could be matched to treatment arms, and only 33 patients (about 7%) were actually treated. Following expansion of the trial, researchers expect to match about 20% of patients to treatment arms.
It has also been shown that drugs that are effective on one cancer may not work on another despite a common genetic mutation. For example, BRAF inhibitors put the brakes on melanoma in patients with the BRAF mutation, but have little effect on BRAF-positive colorectal cancer.
Lex Eggermont, President of the Gustave Roussy Cancer Institute in Paris, warns that the promises of genetic targeting are being oversold. A full molecular portrait – RNA and DNA sequencing and comparative genomic hybridisation (CGH) – will probably identify genetic targets in 50–60 of every 100 patients, he says, but he points out that only half of these targets currently have drugs available. For the 30 patients who can enter a suitable treatment arm, a response rate of around 25% can be expected. “You are left with seven or eight responding patients out of the 100 patients for whom you did all this sequencing and created a molecular portrait.”
For patients who encounter resistance, a similar attrition rate can be expected in a second round of treatment. “You are going to quickly run out of time because the percentages are not going to go upwards, they are going to go downwards. That is not understood by the public because there is an oversimplification in the promises, as if this is a standard approach, whereas it is one big clinical and translation research project.”
In his paper, Denis Lacombe calls for international efforts to conduct these sorts of trials to be pooled. “Histology agnostic trials may become more common in the future, particularly to investigate the effectiveness of therapeutics on rare cancers, but the model still needs to prove its feasibility. It is quite apparent that this kind of trial needs to be based on a strong biological rationale and should not be used to complement weak preclinical data.”





Leave a Reply