
Implement guidelines, adopt what works and reject what doesn’t, focus on cost-effectiveness–there are so many ways cancer care could be improved. Mary Gospodarowicz, believer, pragmatist and ‘raving optimist’, is determined to make it happen.
Implement guidelines, adopt what works and reject what doesn’t, focus on cost-effectiveness – there are so many ways cancer care could be improved without waiting for the next scientific breakthrough. Mary Gospodarowicz, believer, pragmatist and ‘raving optimist’, is determined to make it happen.
Last year, the United Nations General Assembly met to set a new international agenda for non-communicable diseases, including cancer. It was only the second summit of its type with a health focus, and the global health leaders who attended heard that these diseases – which also include diabetes, heart disease and others – are growing at an ‘astonishing’ rate in low- and middle-income countries.
Special mention was made of the economic burden of cancer, which had been flagged up by a World Health Assembly resolution on cancer prevention and control in 2005, prompting the World Health Organization to embark on a cancer control strategy, together with its cancer research body, the International Agency for Research on Cancer (IARC).
Welcome though these developments are, what is remarkable is how long it has taken the major international agencies to recognise the global scale of cancer, and how much responsibility continues to lie with the Union for International Cancer Control (UICC), the long-standing global non-governmental organisation. As its incoming president, Mary Gospodarowicz, a radiation oncologist and medical director at Princess Margaret Hospital in Toronto, explains, the UICC is the only international cancer organisation that aims to bring together the wide variety of players “needed to achieve real improvements on the ground”. They include not only cancer control agencies such as the Centers for Disease Control in the US, Cancer Care Ontario and the Cancer Council of Australia, but also all the professional organisations such as ASCO, ESTRO and ECCO; cancer institutes such as Dana Farber in Boston, Tata Memorial Centre in Mumbai, National Cancer Research Centre in Japan; NGOs such as the American Cancer Society and Association of European Cancer Leagues; plus centres and organisations in low- and middle-income countries such as the Ocean Road Cancer Institute in Tanzania, Nigerian Cancer Society, National Cancer Institute in Chile and others.
“It’s difficult to lead such a diverse organisation,” she says with much understatement. “There is so much need. But following the UN summit we have a big opportunity, now that everyone is recognising that cancer is not only about research and new knowledge but also about applying what we know to trying to improve outcomes worldwide. I’m passionate about getting UICC engaged in promoting what is now called ‘implementation science’ – helping to improve cancer control in a cost-effective way that is appropriate to existing country resources.”
The UICC is also in a special leadership position, because it is able to take a more political standpoint than governmental organisations such as the WHO, which is part of the UN, adds Gospodarowicz. “We can, for example, push governments to commit more funds to cancer. And we have a long-standing reputation around the world; our brand is our biggest asset. We also have a tremendous network of volunteers who contribute their expertise without any expectation of financial compensation.”
The challenge, she says, is how to move UICC’s agenda towards the practical ‘delivery side’ outputs that can really make a difference, and that is not proving to be at all easy. As she points out, the UICC itself has only recently begun to change to a more modern organisation with a vision to attract the right partnerships to determine, and help roll out, what works in cancer control.
“Our core mission hasn’t changed – to eliminate cancer as a major cause of death and suffering – and we produced our own set of targets for 2020, with the World Cancer Declaration. These are, however, very broad and cover the full spectrum of cancer issues.”
The organisation, she says, is now trying to take a more targeted approach. “In the past few years, we have segmented our constituency to talk to different groups such as cancer control agencies, advocacy organisations, research and treatment organisations and patient support groups, and identified priorities across three main activities – advocacy, ‘convening’ and programmes. We have been very good at advocacy – we are known as the voice of cancer globally, while convening is about having meaningful congresses and meetings to preach our cause. And we are focusing on a number of specific programmes.”
Those programmes include My Child Matters, an initiative to boost paediatric cancer cure rates. “A good way to convince people about the value of cancer work is to cure children – the treatments are often inexpensive and effective and kids will go on to live long lives and it is all highly emotional.” Another important programme is the Global Access to Pain Relief Initiative (GAPRI), run jointly with the American Cancer Society, which is attempting to increase the use of opioids to tackle the huge burden of pain suffered in many countries. The third project highlighted by Gospodarowicz focuses on increasing awareness and resources for cervical cancer. It almost goes without saying that tobacco control is also a major concern and needs constant attention as the most important focus for cancer prevention.
There are plenty of other projects, as set out on the UICC’s website, but Gospodarowicz is the first to point out that the organisation has limited resources, and a reorganisation to improve its impact on the delivery side is in its early stages. The UICC, she says, has a current budget of only about $10 million and a staff of about 30 based in its office in Geneva.
It was not until 2006 that the major push to modernise UICC started, due to the efforts of John Seffrin, then UICC president and chief executive of the American Cancer Society. What’s happened since is a more streamlined approach for priorities and programmes, a radically different model for the two-yearly congress, and an injection of new blood into the Geneva HQ.
 This year’s world congress takes place in Gospodarowicz’s home country, Canada, in Montreal – the third conference held under the new model, following those in Geneva, Switzerland (2008) and Shenzen, China (2010). There are also yearly World Cancer Leaders meetings.
This year’s world congress takes place in Gospodarowicz’s home country, Canada, in Montreal – the third conference held under the new model, following those in Geneva, Switzerland (2008) and Shenzen, China (2010). There are also yearly World Cancer Leaders meetings.
Engaging the right mix of professionals, politicians and patient advocates she sees as critical, and while the internet will become a growing force in communication, meetings focusing on implementation and the patient agenda are now the priority, rather than medical topics, which tended to dominate in past years. “We don’t need experts talking about new breast cancer drugs or radiation treatment for prostate cancer – that’s being done elsewhere. What we want is people talking about what works in implementing population-based cancer plans, screening programmes, cost-effective treatments and so on.
“We want people talking about what works in cancer plans, screening, cost-effectiveness and so on”
“Part of the problem is that western countries believe they don’t need the UICC because they think they have their cancer control issues figured out. The perception is that the organisation is for developing regions, which in turn don’t want developed countries telling them what to do. What developing countries want is partnership, and they like the UICC because they are equal partners in it. But we must become more relevant to western countries, otherwise we become just another missionary organisation.”
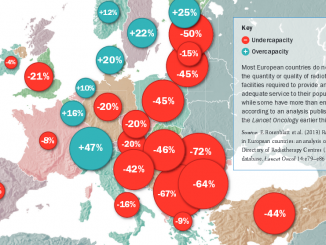
By no means have developed countries worked out all their cancer issues, she adds, noting large variations in care – particularly in remote areas – high costs, and outcomes that in general are not all they could be. “The barriers to good cancer care are not necessarily just about money – some rich countries spend a lot and worry about sustainability of their systems, which is an incentive for them to engage with the UICC.”
A number of professional societies, she adds, have been uninterested in the work of the UICC because of their focus on new, expensive treatments and the inward-looking protection of their members’ interests, an attitude she counters in a typically robust style: “My message to colleagues is: get to the table – it’s not about you, it’s about the patient. There are plenty of doctors who work in NGOs and health ministries who do work with us. We want the UICC to be broad enough to include all involved in cancer.”
Meanwhile, at the UICC’s Geneva HQ, a number of new people have joined in full-time capacities, including a new chief executive in 2009, Cary Adams, who came from the banking sector. “We certainly felt we needed a more business-like approach in the office and in our relationships with other organisations. He refreshed the Geneva team and brought new talent to the UICC. There is new energy in Geneva and while the new aggressive agenda can create some tension, it is a creative tension.” The UICC’s board has also been going through a refresh, and nearly 80 people have been nominated for recent vacancies, which is a very encouraging sign, she adds.
At stake, Gospodarowicz says, is the opportunity to do much more immediately with existing knowledge – “achieving the achievable” as she puts it. “Even with no new discoveries we could increase cancer survival by at least 20%. We know so much more now about prevention and early detection – who would have thought 20 years ago that cervical cancer was induced by a virus, for example?” A recent Lancet Oncology review found that one in six cancers worldwide are caused by viral infections.
“People complain that the outlook for cancer is not good – but in the US, incidence and deaths are going down and the warnings that new conditions and drugs will bankrupt us just has not happened. I remember when AIDS came to Toronto; people said the healthcare system would collapse. It didn’t. In the 1980s some said new drugs for prostate cancer would bust the budget. Not so. I’m known as a raving optimist – and I think any cancer doctor who is not should get out of the business. The last thing a patient needs is a pessimistic cancer doctor.”
Such energy and sense of urgency can make some people in well-established organisations uneasy, she admits. “Change in a worldwide organisation is delicate, but you have to take risks to move forward.”
Her own way to the presidency was paved by high-level success in her Toronto base together with her long involvement with the development of the TNM cancer staging classification – the globally recognised system for staging cancers, which has long been a UICC project and gained the organisation strong recognition.
She was born in Poland and started medical school in the country before moving with her family to Toronto, where she completed her MD. She went into oncology simply because a job came up – Canada was then short of trainees – and Gospodarowicz went on to become a clinical oncologist, with board certification in internal medicine, and both medical oncology and radiation oncology. She chose to practise in the latter.
The first ten years or so were spent juggling family life with her career. “It was very important for me that I had a good home–work balance,” she says, adding that Princess Margaret Hospital, the cancer centre where she has spent her career, was at the leading edge of radiotherapy for a long spell. “I worked with some amazing people and we had great opportunities to carry out clinical trials and international work. Progress in radiotherapy has been so rapid – today I don’t do anything the way I used to when I started out.”
Gospodarowicz is now heavily involved in administration, being not only medical director of Princess Margaret, but also heading radiation medicine, chairing radiation oncology at the University of Toronto (she is now at the end of a 10-year spell) and holding the post of regional vice president for Cancer Care Ontario. She was instrumental in putting the case for modernising radiation oncology when it was clear Ontario risked falling behind.
In a textbook example of how to put a case to decision makers, she and her colleagues drew together the evidence for patient need, the optimum level of new technology, and where the field was heading. “They listened and saw the clear evidence, say, for IMRT for head and neck cancers in improving quality of life, which was a starting point for setting targets for patients treated with new equipment. We went from being several years behind to the forefront by lining up the funding and the right people – such as recruiting a world-class medical physicist, David Jaffray – at the right time. Together we led tremendous change. It was very satisfying.”
“We went from being several years behind to the forefront by lining up the funding and the right people”
Today Princess Margaret has one of the world’s largest radiation oncology programmes, she adds. The total numbers are impressive – over 40 radiation oncologists, 50 medical oncologists, 60 cancer surgeons, and 18,000 new patients a year, mainly from the Toronto area. It is also the largest oncology training centre in Canada.
Gospodarowicz talks excitedly about the latest research and technology agenda at Princess Margaret and in Toronto, such as a major stem cell and a regenerative medicine programme. While stopping uncontrollable cancer cells from developing is one aim, using normal stem cells to repair damage from therapies is another. TECHNA, a new institute for the advancement of health technology created by David Jaffray, and associated with the University of Toronto, aims to bring technologies such as image guidance, nanotechnology, information technology and robotics to healthcare. “It is one of the few such projects in the world and it is very exciting,” she says.
Advances could also impact on intractable problems in her own fields of prostate cancer and lymphomas, such as new image-guided treatment approaches. Princess Margaret has a good track record, she adds, in redefining treatment standards, having for example persisted with work on stopping radiotherapy for stage I testicular cancer and opting instead for surveillance, which is now widely accepted. Another challenge is how to assess the long-term outcomes typical of diseases such as Hodgkin’s, which is a particular interest for her. She is especially proud of her long-term participation in international cooperative group trials, three of which – on prostate, bladder and Hodgkin’s – were well-received last year.
As a senior director in cancer care, she has come to some pragmatic views about the organisation of care, particularly among doctors. A multiple-trained specialist herself, she feels that the lines between specialties are becoming more blurred. Interventional radiologists, she feels, are closer to surgeons than to other radiologists, while in smaller centres patients may be better served by surgeons who are ‘dual trained’ in surgery and chemotherapy, rather than having care provided by two separate doctors – surgeon and oncologist. “It’s good to have one doctor if you are a patient having straightforward chemo- or hormonal therapy,” she says.
Models of multidisciplinary care should not be too rigid, she feels. “We have tried systems where patients are seen by a large number of specialists, and it can be very wasteful. The issue is trust – for example, that I will not miss an opportunity to discuss surgery as a radiation oncologist. But then all team members need a high level of competence – not just superficial knowledge. It’s about being patient-centred and cost effective. I’ve heard that some physicians no longer want to make decisions, and leave them to a group decision at a tumour board, which hasn’t seen the patient. We shouldn’t abdicate our responsibility to a committee.”
“Some physicians no longer want to make decisions, and leave it to a tumour board, which hasn’t seen the patient”
If Gospodarowicz had her way, it would be drummed into medical school students that healthcare is a business and that principles that work in other industries, such as standardisation, improve quality. “If people knew that, they would treat guidelines differently, and not as an infringement on professional freedom. Cancer Care Ontario now collects data on the proportion of patients treated according to evidence, and the adherence to guidelines is suboptimal. But at Princess Margaret, as a research centre, we do have many patients on trials outside of guidelines to create new evidence.”
In fact, she adds, Cancer Care Ontario can now match every patient on its registry with every drug, radiation fraction and surgical procedure, so that outcomes can be reported by tumour site, and staging data are available for 90% of all new cancers. “Although it is new and we are still working on how and what to measure, if we can do it so can others – and it’s just the sort of model that we want to share with UICC members.”
Underlying this work is the fundamental issue of how tumours are classified, and the TNM staging protocol that first brought Gospodarowicz into contact with the UICC, as the Canadian representative on the TNM committee. As she describes, as a young oncologist she had found that there were several different staging systems in testicular cancer, some of them promoted only by a single cancer institute, but a consensus emerged and was translated into the TNM system, which has now been in use for over 60 years.
“I naively thought there was an international organisation responsible for such medical standards,” she says, noting that although the UICC is the custodian of TNM, the effort and continuity depends on volunteer support. “It’s also the case that the other main classification – that of the disease itself, or pathology – has at times had variable international support. While IARC has managed this as a WHO classification, there is no international organisation that has formal responsibility. I found this mind-boggling when I started out as an oncologist.”
This matters a lot because, without strong and consistent support, tumour classification, and TNM in particular, is subject to much misconception and competing interests, Gospodarowicz says, and its value can be diluted. “One problem is that people want to mix the anatomic extent of disease, or stage, with the type of disease (tumour profile), but that’s not a staging classification, it’s a prognostic classification. It is a terminology debate.”
The two can certainly be combined as a prognostic classification – ‘cancer staging’ with ‘tumour profiling’, including also the patient’s characteristics – age, comorbidities and so on, which also determine treatments and outcomes. “This is what people don’t talk about: all prognostic classifications depend on the intervention and what you can apply – a stage I cancer could be fatal or curable. A staging classification tells you how much tumour there is and where it is – you just describe what’s present. I feel passionately that we shouldn’t be discarding a common language for oncologists that’s been around for 50 years.”
It’s not that TNM is standing still – it’s now in its 7th edition and its proponents recognise the need to integrate non-anatomic prognostic factors, but in a way that leaves the underlying values of TNM intact, so it can remain as a worldwide standard for comparing population groups, and stratifying patients into similar groups, which is important, for instance, to allow meaningful clinical trials to be conducted.
Gospodarowicz says the argument is hard to win, with on the one hand, pressures for introducing more complexity from those impatient to push advances in molecular biology into the system, and pleas from cancer registries to actually have a simpler staging classification on the other.
Naturally, medical oncologists generally do not require TNM as a tool for selecting systemic therapy, but TNM is crucial for radiation oncologists and surgeons, who deliver local therapy, she says. TNM has come under particular fire from breast cancer specialists in the West, where a vast majority of patients present with early-stage disease, so TNM alone is not good enough and they need other tools. “But around the world TNM is one of the strongest predictors of outcome – there seems to be an innate desire to change the language,” she says, adding that consensus tends to be an undervalued commodity.
The agenda for the UICC’s Montreal congress is firmly directed at ways to develop consensus and decrease inequality, and Gospodarowicz is hoping that strategies to engage more global leaders will pay dividends. One piece of work she cites that has helped set the agenda is the report from the Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries, of which she was a member, and which was led by Felicia Knaul from the Harvard Global Equity Initiative, and which brought together many of the cancer and healthcare world’s leading lights.
The report, ‘Closing the Cancer Divide… a blueprint to expand access in low and middle income countries’, is extremely important, says Gospodarowicz, because it combines the cause of cancer with economics. “It calculates how much cancer costs and makes the point that countries get richer if they invest in cancer care. It’s a no-brainer that we need to engage with smart people like those at Harvard and amplify their voices.”
The report makes the point that countries get richer if they invest in cancer care
Although rich countries could achieve much more with existing resources, there is clearly a need for more investment in low- and middle-income nations, and the UICC’s role in fundraising is very much on Gospodarowicz’s agenda. “We do have industry financing for some of our programmes, but we need to do much more with other organisations. Targeting philanthropists is difficult – you need a skilled execution body to create the tight proposals that agencies such as the Gates Foundation will act on. We need to capitalise more on our partnerships with WHO and IARC, and others such as GAVI, the global vaccines agency.”
So much more could be done in particular with electronic communications such as mobile health systems (m-health) in developing countries, she says. “The Internet is an amazing equaliser – I now have patients in my clinics who know more than I do. You either fight or embrace it. ICTs [information and communication technologies] should make a huge impact on healthcare and they are part of our new TECHNA institute.”
A project that she encouraged to develop in Canada is ELLICSR, a cancer survivorship laboratory that includes a virtual, online support community. “We don’t know how people will engage with systems like this – it’s still experimental but it’s really not very expensive.”
For Gospodarowicz, change can’t come fast enough, be it in ICT, implementation science or new roles for healthcare professionals – on the last subject she gave a talk last year at the Center for Global Health at the US NCI (itself a welcome new programme) on the need for a rethink on the way that human resources can meet patient needs.
No doubt her family, husband David, a urologist and coroner, and her two children – who have their own rich careers and have not followed their parents into medicine – are well served by all this energy.
Meanwhile, a test of her input into fundraising – and optimism – has recently been set in train by the Princess Margaret Hospital Foundation, which aims to pull in a cool billion dollars (Canadian) for personalised cancer medicine, under the banner, ‘Believe It: we will conquer cancer in our lifetime’. “It’s a huge effort, but we will raise the funds and be successful.”





Leave a Reply