Acute skin reactions associated with radiotherapy can be distressing and can lead to treatment interruption. Anticipating, assessing and managing the problem according to best evidence can make a big difference.
Radiotherapy-related toxicity occurs because of the effect of radiotherapy on normal tissue that divides rapidly, such as the skin and mucous membranes. Acute toxicity occurs during treatment and 2–3 weeks after completing radiotherapy, while late toxicity occurs from weeks to years after treatment.
Skin tolerance was one of the limiting factors in the early days of radiotherapy and can still cause treatment interruptions. It was partly overcome by fractionation – dividing the dose of radiotherapy into several smaller, often daily, doses. Repeated small doses are less damaging than a single fraction with the same total dose. However, despite fractionation there are still problems with skin tolerance, and it remains a reason for treatment interruptions, which can negatively affect treatment outcome with radiotherapy.
Acute skin reactions
Acute skin reactions to radiation are very common, affecting 80–100% of patients treated with adjuvant or curative radiotherapy. Most patients have mild reactions with limited impact on their quality of life. However, some patients, particularly those having radiotherapy to the head and neck or pelvic area, experience more severe reactions. These are associated with symptoms including pain, itching and infections, and in the worst cases lead to treatment interruptions.
Epidermal skin cells are continuously shed from the skin surface and new skin cells are produced in the basal layer below the epidermis. At four to five weeks into radiotherapy, the production of new cells is reduced, and it stops altogether if treatment continues. Skin cells keep peeling off from the surface, with no new cells produced below. In the end, the whole of the epidermis can be lost, and moist desquamation occurs, with the basal layer and dermis exposed. It takes a few weeks after treatment ends before the process of skin cell growth and turnover returns to normal and the skin can heal.

Acute radiation skin reactions occur (see figure above), initially as erythema, ranging from light pink to dark red skin. If the reaction continues, dry desquamation occurs in which the skin appears broken. The next stage is moist desquamation, which is likely to cause infection. In very rare cases nowadays the reaction continues to necrosis.
Risk factors
Risk factors for acute radiation skin reactions include factors related to the treatment itself, to other treatments or to the patient.
Radiotherapy-related factors
Radiotherapy-related factors include dose (the higher the dose, the higher the risk), overall treatment time, volume treated and radiotherapy technique. Using intensity-modulated radiation therapy (IMRT) reduces the risk of severe skin reactions, while the risk is increased by using bolus (material applied to the irradiated area to adjust the dose received at depth and on the skin surface) or by boosting the dose to a specific part of the irradiated area, or using an immobilisation device.
Factors related to other treatments
There may be risk factors related to previous or concomitant chemotherapy, hormone therapy, or targeted therapy. Data from studies are conflicting, however. Some studies show these treatments to be risk factors, while others do not.
Patient-related risk factors
Quite a few studies show high body mass index (BMI), as well as smoking, to be risk factors for acute radiation skin reactions. Age, skin type, genetic variation, comorbidity and alcohol consumption may be risk factors, but the evidence for this is weak.
We published a study on 390 women with breast cancer who were treated with adjuvant radiotherapy after mastectomy, chemotherapy and/or hormone therapy according to guidelines. Their skin was assessed using an assessment tool (RTOG/EORTC scale) and patients reported symptoms.
Data were also collected on health-related quality of life, sleep disturbance and clinical factors including smoking status (measured by carbon monoxide in expired air), BMI and treatment data (The Breast 2013, 22:634–638).
Results showed that 21% of women had severe acute radiotherapy skin reactions at follow-up, 10 days after radiotherapy. Total radiotherapy dose, high BMI, older age and smoking were statistically significantly associated with severe acute radiotherapy skin reactions. High BMI (P<0.001) and smoking (P=0.027) showed the strongest associations. Women who smoked had twice the risk compared to non-smokers. Patients with severe acute radiotherapy skin reactions reported higher levels of pain and increased problems with sleeping.
Management
Research over the last 10 to 15 years has shown that few, or even no, skin care products are effective in preventing or reducing acute radiotherapy skin reactions. A lot of skin products are used that have not been evaluated, and there is wide variation in practice, with many centres using local remedies that have not been tested.
Basic strategies, such as keeping the skin clean with soap and water, seem to be more helpful than particular creams. The goals for skin care are to:
o Keep the skin clean
o Control pain
o Provide comfort
o Avoid friction and trauma from clothes, weather etc
o Prevent infections.
Measures that can help with skin care include pain management and good nutrition to support wound healing. Smoking cessation is one of the most important measures a patient can take to reduce their risk of severe skin reactions. It is important to be careful with sun exposure, to maintain good hygiene and to avoid skin care products just before treatment. Patients should not use make-up on the irradiated area while having radiotherapy, and should use electric rather than manual razors.
What skin care products should patients use?
First of all, patients should use soap and water for washing the skin. Several studies show that soap and water are better than using water alone, because this is associated with higher risk of moist desquamation. The type of soap is not important, but a mild soap is preferable, and highly perfumed soaps should be avoided.
Most creams that have been tested, including those containing Aloe vera or camomile, show no effect. Conflicting results have been seen with creams containing hyaluronic acid, topical steroids (although many centres use these) or calendula. A recent small study showed that olive oil reduced the risk of severe skin reactions (Int J Clin Exp Med 2015, 8:11000–06), while others showed some effects with a sandalwood and turmeric-based cream (Br J Radiol 2014, doi: 10.1259/bjr.20130490) and with a boswellia-based cream (Eur Rev Med Pharmacol Sci 2015, 19:1338–44).
There is a question about whether to use a skin cream or not. At least one study has shown a difference between patients who used a skin cream and those who did not (Radiother Oncol 2004, 73:153–162). It does not hurt to use a skin cream, and I think it can provide a way to keep the skin soft and intact for longer, although there is limited evidence on this.
One of our studies compared calendula cream (marigold extract) with aqueous cream – the standard care at our centre – in 420 patients with breast cancer who were randomised on a blinded basis. The patients’ skin was assessed using the RTOG/EORTC scale, and they were asked to report symptoms. Patients were also asked about their experiences with the skin creams. Results showed no statistically significant difference between the two creams, with slightly higher severe reactions with calendula cream, which was more difficult to apply and more expensive than aqueous cream (EJON 2013, 17:429–435).
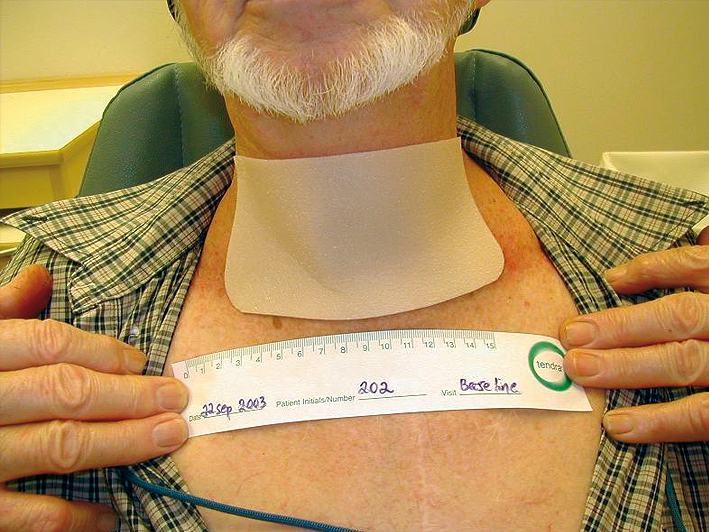
Courtesy of Lena Sharp
Use of topical steroids is a hot topic. There are conflicting data, with some studies showing a reduction in itching and erythema, but no reduction in pain or moist desquamation, which are two major problems (Int J Rad Oncol Biol Phys 2011, 79:1460–66). One study has shown improved quality of life by using topical steroids from the outset of radiotherapy, but there were very few severe skin reactions in the placebo group (Int J Rad Oncol Biol Phys 2014, 90:748–755). There are no data on long-term effects of topical steroids on irradiated skin. I would recommend against using topical steroids for all patients, but to assess the risk factors for each patient, and use steroids if appropriate. Soft silicone dressings can help to prevent trauma and friction (see figure above). In most cases these can be left on during radiotherapy, although this should be discussed with the radiotherapy team.
There may be a risk of increased dose to the skin surface, if the dressing is left in place during radiotherapy, but this is not clinically relevant. A problem with these dressings is that they are expensive, and are therefore not available to all patients.
Question: Do you think intensity modulated radiotherapy (IMRT) is more effective in the prevention of acute radiation skin reactions than 3D radiotherapy?
Answer: Yes, I think so. But a lot of factors have to be taken into consideration. Using IMRT for all breast cancer patients would increase treatment time, which may cause problems. However, I think it would definitely be better for the skin.
Question: Is the pH of soap relevant? If yes, what is the evidence on optimal pH for soap?
Answer: It doesn’t seem to matter. It seems to work with any mild, preferably perfume-free soap. I think we focus too much on things like that.
Question: Is steroid therapy really not applicable?
Answer: You can definitely use it, but I don’t think you should recommend it for all patients from the start of therapy. There are not a lot of data on long-term use. Consider using it if a patient develops a severe skin reaction early in treatment, or if they have other risk factors. There are studies showing it might improve quality of life and itching, but my advice is that steroids are not for general use.
Question: If you are trying to solve itching, would you be better using an antihistamine rather than a topical cream, if appropriate for a patient?
Answer: Yes. Good idea.
General recommendations
Patients with erythema should wash the skin with mild soap and water daily and apply a perfume-free lotion. Dry desquamation is treated in a similar way, washing with mild soap and water daily, in addition to avoiding friction and trauma, such as rubbing of shirt collars. Silicone dressings or silver dressings can be used to cover the irradiated area to reduce friction, although silver dressings should not be left on during treatment. Moist desquamation is treated in the same way, ensuring that any infections are treated with antibiotics.
Combined treatments: radiotherapy and targeted drugs
Targeted drugs can cause skin rash, and it is important to consider the combination of this with the skin toxicity associated with radiotherapy. One of the problems with combined treatments is that more severe skin reactions can occur, particularly with higher doses of radiotherapy. The patterns of skin reactions to targeted drugs also differ from those associated with radiotherapy. Skin toxicities from targeted therapies can start much earlier, and there is currently limited understanding of the late toxicities with the combination with radiotherapy, because it has been used only relatively recently.
These skin problems need to be treated with antibiotics immediately, because it is even more important to avoid treatment interruptions for patients on combined treatments. Many patients with colorectal cancer have targeted therapies, and are advised to cover up the skin reactions to these drugs with makeup. Patients receiving radiotherapy for head and neck cancers, however, should avoid makeup on areas of irradiated skin. There is limited evidence on management, but a recent literature review in head and neck cancer treated with radiotherapy plus chemotherapy or EGFR inhibitors provides some information (Crit Rev Oncol Haematol 2015, 96:167–182).
Assessing skin reactions to radiotherapy
Many of the assessment tools currently used are not validated. Assessments should include, or be combined with, patient-reported data, because the most important factor is not how red a patient’s skin is, but how the reaction and symptoms affect them. You should assess the patient’s skin before, during and after radiotherapy to enable comparison.
It is important to consider inter-observer variability. We tested two different tools used independently by two very experienced nurses in patients with breast cancer, and found inter-observer agreement of 50–60% (EJC 2011, 47 2665–72). In some cases the difference was two steps on the measurement scale. When we explored the reasons for the difference, we found that many nurses assess the redness differently. Education is essential and, after our study, we held workshops with all of our staff on the use of skin assessment tools, and found we could increase inter-observer agreement to 90%.
Question: What online assessment tools do you recommend?
Answer: It is important to see whether your department is already using an assessment tool and to use that, particularly if the department is using it in research. A useful measure for assessing patient-reported symptoms, and for staff to assess the skin, is the RISRAS scale, and we have used the RTOG/EORTC scale, which has been widely used in Europe. However, with any measure it is important to include patient-reported symptoms. A useful overview of assessment tools for acute radiation skin reactions has been published in the Clinical Journal of Oncology Nursing (vol 15, pp 481–492).
Question: What about areas of the skin where you can’t apply dressings, such as for patients treated for rectal or gynaecological cancers, who can develop quite severe skin reactions? How should these patients be managed?
Answer: This is really difficult, but should include the same management as for other areas of the skin. We have used silicon dressings in these situations. They will fall off and need to be changed, but would need to be changed several times in these areas anyway. There are sprays and other preparations that could be used after the treatment period, but not during treatment. Gauze may be placed in skin folds, to try to avoid skin–skin contact. A hand shower should be used to keep the skin clean.
Question: Given the variation in practice between different centres and the lack of evidence for one product compared to another it is difficult to develop institutional guidelines. Do you have any recommendations on this?
Answer: I think it is important to keep it simple. Although there is a lack of evidence, that does not mean a product is harmful, and if an institution finds something works, then that is fine. Use any type of moisturiser that works and is available locally. One approach is to ask the patient about the moisturiser they normally use, and recommend they continue, as long as it is perfume-free. I think we put too much focus on the type of cream, but this does not really matter.
Question:. Is there any evidence on the use of sucralfate in ulcerated lesions in radiodermatitis?
Answer: A very well-designed UK study showed no evidence of benefit in colorectal and breast cancer patients (Radiother Oncol 2004 73:153–162).
Question: Is there any recommendation on when patients should start applying skin care products – before or after onset of the skin reaction?
Answer: There is no strong evidence, but I would recommend starting when treatment starts. This also provides a good way of checking the skin. The skin reaction will occur anyway in response to radiotherapy, but it is important to help the patient continue with treatment so they don’t have interruptions.
Take home messages
Most patients experience acute skin reactions from radiotherapy, mostly mild to moderate Patients should be advised to keep their skin clean with soap and water. A lot of remedies are used by di erent centres but with little or no evidence. Using a simple moisturiser could be helpful; however, there is no strong evidence in favour of any particular type of skin care product. Smoking is the most important patient-related risk factor for skin reactions, and starting radiotherapy provides a useful teachable moment to help people stop. High BMI is also a risk factor.