Prioritising collaboration over self-interest is the way to learn about who gets the best from which treatments in the complex world of advanced prostate cancer. Silke Gillessen talked to Simon Crompton about how she is trying to bring people together to make it happen.
Prostate cancer is lethal. With medics increasingly aware of the prevalence of indolent prostate cancer and the need to avoid overtreatment, there is a danger that this important reality gets overlooked.
Silke Gillessen is a Swiss medical oncologist who has spent the last 15 years working with, and trying to improve the lives of, men with advanced prostate cancer. The instigator of a ground-breaking consensus conference held in 2015, she has established herself over the past decade as a leading force in getting better treatment for advanced prostate cancer higher on the international research agenda.
And when I talk to her, the message she wants to convey to all the cancer community is that the deadly seriousness of prostate cancer is easily forgotten.

“It is one of the most misunderstood cancers,” she says. “A lot of people still think: ‘Oh yes, prostate cancer is smouldering, and it affects older men so there are rarely any problems. But that is not true. In most Western countries it is the second most common cause of cancer death in men, and as soon as someone develops metastases, it is most of the time lethal. I don’t think this is something that has reached the general medical community.”
Nor, she says, is there sufficient appreciation that age is not what it used to be. Effective novel diagnostics and treatments for older populations should be a priority because more people over 65 are active and working than even 20 years ago. More emphasis on prolonging and improving life in elderly patients is urgently needed.
This may help explain why advanced prostate cancer is not well understood. It has undoubtedly been neglected, says Gillessen. The situation has parallels with care for other advanced cancers. For example, the new Global Status of Advanced/ Metastatic Breast Cancer report, published by the European School of Oncology in conjunction with Pfizer, reveals there are still substantial gaps in care, lack of access to resources and support, and poor treatment outcomes for women with advanced breast cancer. But while filling those gaps is now well and truly on the international agenda in advanced breast cancer, the same cannot be said of prostate cancer. Gillessen wants to make things happen.
“We were surprised how many
other questions and topics there are
where there is no high level evidence or data”
She remembers how, three years ago, she was sitting having a coffee with her colleague, Aurelius Omlin, at the Kantonsspital, St Gallen, in Switzerland, where she is Senior Oncology Consultant specialising in genitourinary tumours and head of the Oncology Clinical Trials Unit. They started discussing how the arrival of new treatment options in the past five years, such as abiraterone and enzalutamide, was improving survival and quality of life for men with metastatic prostate cancer, but how difficult it was to counsel patients about the best sequence of approved treatment options in the absence of reliable evidence on best choice of first-line therapy.
“And when we started looking deeper into it, we were surprised how many other questions and topics there are where there is no high level evidence or data,” she says.
Her response was to organise a major meeting, bringing some of the world’s top prostate cancer experts to St Gallen – an event analogous to the international Breast Cancer Consensus Conference that has taken place there since 1978. The objective was to acknowledge uncertainty, yet find agreement on best clinical practice nonetheless.
“If you don’t have good evidence, the second best you can have is consensus from experts in the field, so that’s why we did it.”
The result was the inaugural St Gallen Advanced Prostate Cancer Consensus Conference (APCCC), held in March 2015.
It resulted in an influential set of expert recommendations on the daily management of advanced prostate cancer. It also cemented Gillessen’s reputation as someone who is bringing change in the treatment and care of people with advanced prostate cancer by bringing people together, encouraging discussion and confronting some of the traditional boundaries that prevent progress.
Getting knowledge out there
“Maybe it’s because I’m Swiss, or female, or both, but I don’t think we should compete. What I’m for is a unified community that really tries to do the best for our patients. I think we could advance better if we worked as a community and this is particularly important in prostate cancer, where multidisciplinary work is crucial in my eyes.”
Interestingly, the consensus conference came up with some remarkably clear recommendations for what clinicians should do, even given the uncertainty surrounding existing evidence. For example, there was consensus (i.e. at least 75% agreement) among the 41 experts that it was wrong to treat men with metastatic castration-sensitive prostate cancer with high doses of bone-targeted drugs like bisphosphonates or denosumab to reduce the incidence of skeletal related events.
“It is not recommended because there are side effects and no proven benefits,” says Gillessen. “Two big trials evaluating zoledronate in this situation show this. But when I’ve given talks, I’d say 50–70% of oncologists or urologists do this. One of the reasons is that there is so much pressure from pharmaceutical companies.”
“If you haven’t got centralised medicine,
then let’s get the knowledge out there,
so that people know where to look and who to call”
There are other examples of common practice which the experts disapproved of – for example, stopping life-prolonging treatment in men with castration-resistant prostate cancer on the basis of a PSA rise alone. “It’s important that these messages get into the cancer community,” she says. The areas of agreement were published in the Annals of Oncology in June last year.
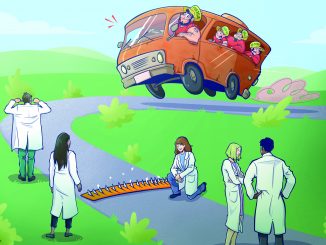
“If findings are to have an effect on patients, it can only be done by spreading knowledge. A lot of men don’t get the right treatment, or don’t have access to leading treatments. Treating physicians in many countries don’t have a lot of experience in treating men with advanced prostate cancer, because they are not in specialist centres and are sometimes only seeing a few prostate cancer patients a year. If you haven’t got centralised medicine, then let’s go for the second best and get the knowledge out there, so that people know where to look and who to call.”
Uncertainty remained in some areas of discussion at St Gallen. The experts could not agree, for example, on the optimal dose, schedule and duration of osteoclast-targeted therapies. And there was also little agreement on the best way of diagnosing and treating oligometastatic disease.
But these areas are as important as those where there was agreement, argues Gillessen. They will become a focus of discussion at future St Gallen advanced prostate cancer consensus conferences – the next is planned for March next year (www.apccc.org).
Finding answers
They also provide a research agenda for advanced prostate cancer. One important area where there is considerable uncertainty, for example, is in the use of imaging to stage and monitor prostate cancer. There are new sophisticated techniques, using PET/CT or whole body MRI, but research correlating better imaging with better clinical outcomes is missing. Research on patient quality of life during and following treatment is also lacking. “A lot of my patients tell me that their quality of life is more important to them than quantity of life, so there should be much more focus on it.”
Why are there such gaps in research on advanced prostate cancer? Gillessen isn’t sure it has anything to do with advanced disease somehow being less ‘sexy’ than other fields. She says it has more to do with regulations getting in the way of important international trials that don’t involve new drugs. “The administration is crazy, and it’s probably got worse over the past 20 years. It’s a political issue: academic trials have to carry out exactly the same administrative work as the pharmaceutical industry, but we don’t have the resources. A lot of it is over-regulated and I’m not sure it’s really helping the patient.”
Treating advanced prostate cancer
□ Localised prostate cancer is normally treated with active surveillance or surgery and/or radiotherapy.
□ If the prostate cancer has advanced beyond the capsule of the prostate gland or has metastatised, the treatment is likely to include hormone therapy.
□ Prostate cancers need testosterone to grow, and hormone therapy, administered by tablets, injections or surgical castration, shrinks or slows advancing tumours by lowering levels of testosterone. This is called androgen deprivation therapy (ADT).
□ ADT only holds prostate cancers for so long. Tumours that are still responding to hormone therapy are called castration-naive. Tumours that are no longer responding are castration-resistant.
□ Once a cancer has become castration-resistant, there are still treatment options. There is an increasing number of novel drugs, but the best options, combinations and timings are still debated.
Yet Gillessen refuses to dwell on the fact that her field has not attracted the research funding or professional focus that it should have in the past. “Maybe it has been neglected, but a lot of pharmaceutical companies and some charities are interested now, and there are now a lot of phase III trials and it will be improving more and more in the coming years.”
Remembering her own professional beginnings, she knows how far things have come. The frustration of seeing how little there was available for advanced prostate cancer patients proved a driving force in her career.
Making a difference
According to her mother, Gillessen decided she wanted to become a doctor while accompanying her brother to his vaccinations at the age of four. Her parents – both research chemists – always emphasised to her that anything was possible in terms of a career, and in 1992 she qualified as a doctor at the University of Basel. She started in general medicine, then moved to internal medicine at the Thurgauer Schaffhauser Höhenklinik hospital, Davos, Switzerland, where she worked with her first prostate cancer patients.
“I still remember one or two patients that were very close to my heart, but we didn’t have anything for them apart from hormonal treatments. It was very frustrating. You felt this connection with patients and you felt you should be able to do something. But there was this big hole. It really started from there.”
So although Gillessen spent time as an immunology researcher at Roche in the United States and in the Dana-Farber Cancer Institute in Boston, she missed working with patients and she returned to Switzerland to work in oncology, first in Basel and then in St Gallen. She became a consultant in oncology and haematology at the Kantonsspital in 2001 and senior consultant in 2008.
“I appreciate what you learn from prostate cancer patients –
how they accept what is happening and handle it”
The patients she has treated have been one of the biggest influences on her throughout her career. “You have the opportunity to develop long-term relationships with people who have cancer,” she says. “I appreciate what you learn from prostate cancer patients – how they accept what is happening and handle it.” She also, she says, simply gets on well with men, both as work colleagues and patients.
That has proved an asset working in the men’s world of genitourinary medicine. But Gillessen has never seen her gender as a barrier. Her mother was an inspiration: she was one of only a handful of women in her generation who obtained a PhD. But also influential were other women physicians who specialised in genito-urinary oncology, and excelled.
“Seeing people like Maha Hussain [Professor of Medicine and Urology, University of Michigan, USA] or Cora Sternberg [Chair, Department of Medical Oncology, San Camillo Forlanini Hospital, Italy] give fantastic talks at ASCO and European conferences, at a time when there weren’t many Swiss women in academic research, really showed me you can do it if you’re a woman. They were role models.”
Tackling the ‘who needs what’ question
Today, the research priority has to be finding better markers to predict the course of prostate cancer and help determine who will respond best to which treatments, she says.
“We need biomarkers which tell us whether, when someone has a PSA relapse after curative treatment, it’s just local or systemic. We need biomarkers to tell us which are the really high-risk prostate cancers that require multimodality treatment, and which are the ones where one treatment is likely to be enough.”
“We need real predictive factors saying who is responding to hormone treatment, who is responding to chemotherapy, who is responding to PARP inhibitors. It is a very important challenge.”
She has worked in the field herself, having patented a new method of determining potential biomarkers and drug targets, together with colleagues at the Swiss Federal Institute of Technology (ETH) Zürich and the Kantonsspital St Gallen. And there is much hope elsewhere, she says. Lung cancer has shown the way forward, with new predictive factors identifying which mutational changes drive disease and are targetable.
In advanced prostate cancer, there is promise in AR-V7 testing, which seems to predict whether patients with castration-resistant prostate cancer will respond to novel endocrine agents such as enzalutamide and abiraterone. And the work of Johann de Bono at the Institute of Cancer Research, London, on alterations in DNA repair genes predicting response to PARP inhibitors, looks very promising. “There is a lot of light on the horizon,” she says.
Tackling the access question
One of the focuses of her own research has been finding cheap yet effective treatments that might be made widely available in resource-poor countries – and in poor populations in higher income countries such as the United States. But finding financial support has been difficult.
For example, a trial at St Gallen has begun looking at the use of platins (as opposed to more expensive PARP inhibitors) in men with prostate cancer with mutations in their DNA repair genes. There are already some data suggesting that platins are effective, and they are cheap because they are out of patent. But because platins are generic, pharmaceutical companies are not interested in testing them, and it has taken “a very long time” to find trial funding. Gillessen looks to the UK, where funding from the Medical Research Council means that purely academic trials of ‘not sexy’ drugs can get funding.
“I think there are a lot of old drugs out there that are interesting and would be cheap, but it’s very difficult to run trials,” she says. “It’s about providing global access to drugs. This is a very important topic in every cancer.” (For more on this problem see: Too affordable: how do we overcome the drug repurposing paradox? Cancer World Sept–Oct 2016).
Similarly, she is involved in trials investigating the use of metformin – another very cheap drug – in treating castration-resistant and castration-sensitive prostate cancer, with the hope of additionally mitigating some of the adverse effects of androgen deprivation therapy.
She is also involved in planning a trial investigating the benefits of providing commonly available drugs such as aspirin and statins to patients with castration-resistant prostate cancer. This too might help reduce side effects and prolong survival. The research is planned to run under the PEACE initiative (Prostate Cancer Consortium in Europe), a recently established initiative that aims to foster cross-border networks of investigators.
“Health is important, but so is our environment.
We have to try and not be so self-centred,
and think about future generations”
“In the end it all comes back to the fact that advanced prostate cancer is a very heterogenous disease, and we have to find subgroups that respond to certain treatments. We have shown that we can prolong survival, and our patients live longer and better than they did 10 years ago. But we obviously want to improve that further.”
Only collaboration will get answers
Collaboration, and letting go of self-interest, are key to making this happen, argues Gillessen. She has a broad perspective on life: she loves art, classical music, theatre, and mountain hiking with her architect husband. She enjoys good food, wine and conversation with friends who are artists as well as scientists. And she has an acute awareness of the bigger picture. “We are not the centre of the world,” she says. “There are other things too. Health is extremely important, but so is our environment. We have to try and not be so self-centred, and think about future generations.”
Perhaps this wide-reaching outlook is why she can see above narrow professional perspectives, and is determined to keep on promoting equity and the type of constructive pooling of expertise that the first St Gallen consensus conference exemplified.
Pooling expertise
The 2015 Advanced Prostate Cancer Consensus Conference brought together 41 clinicians and researchers from 17 countries to discuss key uncertainties in caring for patients with advanced prostate cancer, with a view to reaching consensus positions to guide clinical practice in the absence of robust evidence. The resulting expert recommendations complement evidence-based guidelines, and will aid discussions between men with prostate cancer and physicians when faced with management decisions. The second APCCC conference will be held in St Gallen on 9–11 March 2017. You can register or find further information at www.apccc.org.
“There are a lot of patients, and a lot of open questions, and there’s room for all of us,” she says. “In small surroundings, with friendly people – like at my hospital – collaborative work works perfectly. But it’s fantastic if you can do that at a higher or international level too, and we’re trying to do that, starting to talk to people in organisations such as EAU, ESMO, EORTC and ESTRO, and trying to do research together on a European level.
“It takes time, but I think it’s more fruitful than competing. It’s not about little kingdoms, it’s about trying to work together, do the best for our patients and make the best use of the resources we have.”