
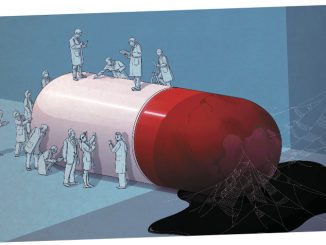
Are dysfunctional relations between academia and industry hindering the process of turning progress in our understanding of cancer into truly effective treatments?
The business model for developing new cancer drugs is broken and needs replacing with more efficient forms of public–private collaboration. This was a key message from the Stop Cancer Now! appeal made to governments and policy makers on February 4th, World Cancer Day. It reflects a growing concern that the relations between industry and academia need to change if we are to translate the impressive advances in our knowledge and understanding of cancer into breakthrough treatments.
This concern was also addressed in an EORTC position paper in January 2013 (EJC 49:1–7). The authors call for a new model of partnership between industry and academia to allow each to play to their “core competencies” to improve drug development by ensuring better integration of standardised, quality-controlled clinical, biological and imaging data into the decision-making process. Are they right? If so, what should the new partnership look like? Cancer World’s Anna Wagstaff put the question to Lex Eggermont, director of the Gustave Roussy cancer institute in Villejuif, Paris, and Bill Hait, global head, Janssen Research & Development.
Lex Eggermont
 We should first acknowledge that our ability to identify targets and develop drugs against those targets is a major scientific breakthrough. Our lack of progress in clinical terms reflects the complexity of cancer. The initial reasoning was that a drug that works against a given target, e.g. mutated BRAF, would work across different diseases defined by that particular target. This would have meant that the old-style pharmaceutical business model of finding ‘blockbuster’ drugs that work over large populations might have remained viable. But this does not seem to be supported by the evidence, because we now know that the organ of origin – the tumour environment – plays an important role, so a BRAF inhibitor that shows a good response in BRAF-mutated melanomas, for instance, shows no such response in colorectal cancers with the same mutation.
We should first acknowledge that our ability to identify targets and develop drugs against those targets is a major scientific breakthrough. Our lack of progress in clinical terms reflects the complexity of cancer. The initial reasoning was that a drug that works against a given target, e.g. mutated BRAF, would work across different diseases defined by that particular target. This would have meant that the old-style pharmaceutical business model of finding ‘blockbuster’ drugs that work over large populations might have remained viable. But this does not seem to be supported by the evidence, because we now know that the organ of origin – the tumour environment – plays an important role, so a BRAF inhibitor that shows a good response in BRAF-mutated melanomas, for instance, shows no such response in colorectal cancers with the same mutation.
The challenge for industry is to find a financial model that can sustain developing drugs that work well in small populations. The challenge for all of us is to find a way to make the science work. The clinical side of the drug development programmes has become far more important, and I think the EORTC is right to focus on the need to ensure better integration of standardised, quality-controlled clinical, biological and imaging data into the decision-making process. The work must be led by medical oncologists and imaging oncologists, because they are trained to have that broad vision and understand multiple tumour types. They have to use all their knowledge about the disease, and programmes must be science driven – with multiple biopsies, multiple evaluation points and multiple investigation techniques, such as functional imaging. Everything has to be worked out in phase I and early phase II, and only if you see convincing and consistent effects will you take a drug into a phase III trial.
Such work can only be carried out at centres of excellence, which have the experience, expertise and infrastructure. These are the centres that, together with industry, will make the discoveries but will also kill many drugs that are not good enough to be moved into later phases. Our dependency on one another is now much greater.
Bill Hait
 A lot of oncology drugs have been approved in the last two years, some of which make a big difference, but there’s no question that we haven’t cured as many cancers as we might have hoped.
A lot of oncology drugs have been approved in the last two years, some of which make a big difference, but there’s no question that we haven’t cured as many cancers as we might have hoped.
I think part of the problem is that we became too enamoured with the technology. The ability to clone genes, express proteins, make crystals, and use those crystals to conduct structure-based drug design became so ‘easy’ compared to the old-fashioned way, that we got carried away. We assumed that as soon as we made a drug against an identified target it would solve the problem. I agree with Lex that it just hasn’t turned out that way, but I don’t think lack of interactions between academic institutions and industry on clinical trials is the major problem – clinical trials are collaborative by their very nature.
I believe the big problem centres on how you translate a fundamental discovery into an active drug. Pharma companies are experts in developing drugs, but have very limited understanding of the biology and pathophysiology of disease. Academia, on the other hand, has very little expertise in drug development, but has very deep expertise in disease. We need to be able to sit down together and look, for instance, at drug resistance in acute myeloblastic leukaemia and ask: what are the drivers of those cancer cells? What are those pathways? What are those antigens? How do we get closer to knowing that this pathway and the targets in this pathway are most likely to have a pay-off in those patients if we could make a good drug?
We should come together in robust and meaningful collaboration bringing our expertise to the table and not be ships passing in the night. A good example is the agreement Stephen Friend negotiated with the Lee Moffitt Cancer Center in Florida, when he was at Merck. Merck funded the setting up a of network of hospitals that would provide Moffitt with tissue samples for cancer genome analysis. It was a very large investment on Merck’s part, and a sizeable investment in time and effort by the Moffitt Cancer Center, but because of that partnership they now have probably more information and data than they could ever have imagined.
An example we are very much involved with is a partnership with the Koch Institute for Integrative Cancer Research at MIT, where we work together on the tumour microenvironment and immunologic microenvironment, which are areas of mutual interest.
 I agree that the big challenge is to understand more about drivers and resistance mechanisms in different cancers, and that requires collaboration. But the elephant in the room is how to get around the intellectual property [IP] restrictions so that the data that is generated can be shared. Once the data is out in the public domain, anybody in this world who has a scientific brain and analytic power can analyse it and come up with ideas. In fact Stephen Friend left Merck to set up Sage Bionetwork, a non-profit organisation that promotes open data sharing, and sets open challenges to encourage interested scientists to focus on particular problems and data sets, to see who can come up with the most discriminatory bioinformatic analytical models.
I agree that the big challenge is to understand more about drivers and resistance mechanisms in different cancers, and that requires collaboration. But the elephant in the room is how to get around the intellectual property [IP] restrictions so that the data that is generated can be shared. Once the data is out in the public domain, anybody in this world who has a scientific brain and analytic power can analyse it and come up with ideas. In fact Stephen Friend left Merck to set up Sage Bionetwork, a non-profit organisation that promotes open data sharing, and sets open challenges to encourage interested scientists to focus on particular problems and data sets, to see who can come up with the most discriminatory bioinformatic analytical models.
Most cancer centres are involved in programmes and partnerships exploring a lot of different avenues and they are creating huge data warehouses. But if we don’t know how to resolve the IP problem around data generating and data sharing, it’s hard to see how you can develop a partnership model that will make it possible to explore all the data that already exists but is locked away.
That said, I don’t think the disappointing performance of targeted drugs can be ascribed entirely to failures at the more fundamental level of research. Resources are being wasted because too many drugs make it into clinical trials without convincing data that they have the potential to make a big difference. I think one reason is that many preclinical programmes are conducted too much in isolation rather being tested in a broader range of models. I often see data presented as very hopeful and promising, and I am totally underwhelmed by what I am looking at. This can be a particular problem with biotechs that have everything riding on the success of just one or two molecules, but it can play a role wherever scientists’ future prospects are linked in some way with the success of the project.
When you analyse data from 20 experiments, it’s easy to focus only on the better results and find excuses for why some didn’t turn out so well. People with a broader perspective on the disease may be more cautious about proceeding until more is understood about the reasons for the inconsistent results. Better collaboration, particularly at the preclinical stage, could ensure a more critical evaluation of the strengths of a particular molecule.
 I agree that the failure rate is too high, but I don’t see the problem as a lack of robust interaction or use of enough preclinical models. Between all of us, we still lack adequate knowledge to predict with greater certainty which drug will work and which will fail. In my experience, teams that work on a compound spend an enormous amount of time working with many molecules and many sites of interaction with the target. These people live and die for their compound and by the time a drug is ready to enter clinical trials there has usually been significant input from external experts on advisory boards. These experts won’t have seen only the good data, because companies tend to seek advice on the areas where they are uncertain, so are more likely to focus on the less convincing data.
I agree that the failure rate is too high, but I don’t see the problem as a lack of robust interaction or use of enough preclinical models. Between all of us, we still lack adequate knowledge to predict with greater certainty which drug will work and which will fail. In my experience, teams that work on a compound spend an enormous amount of time working with many molecules and many sites of interaction with the target. These people live and die for their compound and by the time a drug is ready to enter clinical trials there has usually been significant input from external experts on advisory boards. These experts won’t have seen only the good data, because companies tend to seek advice on the areas where they are uncertain, so are more likely to focus on the less convincing data.
On the issue of IP and sharing data: would things would go better if relations between industry and academia were more open, as Lex suggests, so that everybody could pitch in? It sounds reasonable when you first hear it, but there is also the other possibility of too many cooks spoiling the broth. If I make an observation that I think is critically important, I would be much more interested in finding the best person or people in the world that I can collaborate with on it. It is more manageable, it is not going to create a lot of noise, and I think it would be more productive. Take Herceptin. The discovery of HER2 neu was made by Bob Weinberg at MIT in a cell line that came from a brain tumour. Denis Slamon observed that HER2 neu was being overexpressed in breast cancer and that it portended a very poor prognosis, and Genentech gave Denis Slamon the tools to explore the space of HER2-positive breast cancer. Then some fantastic scientists at Genentech went on to develop Herceptin.
It’s easy to say: let’s ignore IP. But at the end of the day, we have to preserve a pharmaceutical company’s ability to be profitable, so that it will have the funds to reinvest in the important and innovative research that impacts the health and welfare of people in the world. As in all highly innovative industries, IP is essential for this model to work. You have to be sensitive to that.
 The problem is that the model that worked for developing Herceptin has not worked as well as we had hoped for other types of disease, because most solid tumours have turned out to be far more complex, with multiple drivers. But we’re not going to solve the problem if we keep so much data, particularly all the sequencing data, behind closed doors. We have to open up at some point, and earlier than now, to the benefits of the unparalleled analytic power that is around. We should also bear in mind that most institutes where we are working run on tax payers’ money, so the public should have some right of access to the information we help generate.
The problem is that the model that worked for developing Herceptin has not worked as well as we had hoped for other types of disease, because most solid tumours have turned out to be far more complex, with multiple drivers. But we’re not going to solve the problem if we keep so much data, particularly all the sequencing data, behind closed doors. We have to open up at some point, and earlier than now, to the benefits of the unparalleled analytic power that is around. We should also bear in mind that most institutes where we are working run on tax payers’ money, so the public should have some right of access to the information we help generate.
For me, the question is how you can construct partnerships that protect IP rights while still putting a whole lot of raw data on the internet where other people can try their hand at making sense of it. That could be a very technical discussion about where IP starts and where it ends, but if the industry doesn’t open up to more open partnerships and data sharing, I don’t see how it will survive. We can die together or live together, but we will certainly need a big change to live together. If we can’t change the paradigm to create open partnerships and publicly shared data, then I think it will just suffocate. Cancer is too complex to be solved by pharma alone, and too complex to be solved by academic institutions working alone. We have to invite in all the analytical power and infrastructure that is out there.
 That sounds right until you get into specific examples. We’ve had instances where an academic person requested raw data for a particular project. He had good academic credentials and we were about to turn over the data when our attorneys found out that this person had just started a company that was trying to produce a competitor drug. We were about to give that person the raw data.
That sounds right until you get into specific examples. We’ve had instances where an academic person requested raw data for a particular project. He had good academic credentials and we were about to turn over the data when our attorneys found out that this person had just started a company that was trying to produce a competitor drug. We were about to give that person the raw data.
You need to be aware that there are noble people out there who want to do the right thing. Then there are others who may have ulterior motives, and companies need to protect themselves from that.
We came up with an idea a couple of years ago called an I-SPORE (SPORE being a grant scheme run by the US National Institutes of Health). We said to leaders of a couple of universities: we’ll put on the table all of our reagents, capabilities and drugs, in return for you, the academic leaders, helping us understand in greater detail the drivers of a particular type of cancer.
In the end it didn’t come to anything, because it was very hard to reach agreement on some of the details – the usual barriers of how quickly you publish, who gets what credit when you work as a team, royalties, protection of IP. I think it’s basically a good idea and none of those barriers are insurmountable.
Could such an agreement incorporate provision for open sharing of some of the raw data? Quite possibly. Under the proper circumstances, proper investigators opening up the books to raw data could be very useful for both the industry and the investigators, but there has to be some care in doing that. We need to continue to ask these questions and work together to find a solution.





Leave a Reply