
Eurocare, the landmark series of studies comparing survival of cancer patients among European countries, has been profoundly important in focusing attention on the quality of Europe’s cancer services over the past two decades.
Now in its fifth edition, and including data on 21 million cancer diagnoses held in 116 cancer registries in 30 countries, it graphically demonstrates important variations in survival rates, broken down by cancer type, that had previously been hidden. In doing so, it introduced the concept of ‘unnecessary deaths’ – deaths that could have been prevented with earlier diagnosis or more appropriate treatment – and gave ammunition to advocates and politicians to press for overhauls of poorly performing cancer services.
One of its more notable impacts has been in the UK, whose poor showing in the Eurocare-2 studies came as a shock to a country that had always seen itself as ahead of the field in cancer (see Survival of cancer patients in Europe: the EUROCARE study. IARC Scientific Publications No 132). The data showing survival rates for patients in England and Scotland as consistently below the European average were instrumental in prompting the government to introduce a pioneering cancer plan for the National Health Service in the year 2000.
Denmark, another surprise under-performer, reacted in a similar fashion, drawing up its first cancer plan; while in Germany, a certification system for breast clinics was implemented in 2003 partly because poor survival results were identified by Eurocare.
But while the Eurocare studies have undoubtedly fuelled important policy initiatives, questions remain about how far they have actually led to improvements in patient outcomes.
The narrowing of the major survival gap between western Europe and countries of eastern and central Europe during the first decade of the new millennium would appear to show that they have. Yet the underperformance of the UK and Denmark has continued as a notable feature of successive Eurocare studies, up to and including Eurocare-5, published at the end of 2013 (see, for instance, http://tinyurl.com/eurocare-5).
Attempts to analyse why this is happening have focused attention both on the reliability of the data, and on the need for additional comparative data that could help throw light on what lies behind survival differences, to better inform efforts to tackle them. And the hope is that Europe will have its first unified cancer information system in the next few years, with a first step – an interactive visualisation tool of incidence, prevalence and survival – on track for release by the end of 2016 (see box).
ECIS: A cancer information system for Europe
The European Cancer Information System (ECIS) is a joint project of the European Commission’s Joint Research Centre and the European Network of Cancer Registries (ENCR). It aims to provide European countries with a range of indicators that can be compared across registries and over time.
The first aim is an interactive visualisation tool of already published aggregated and anonymous data of incidence, prevalence and survival. But a wider set of possible indicators is already available from the Eurochip project, while others have yet to be developed, and in total could include those shown here.
In essence, the project aims to marry high detail, individual level data from clinics and registries with low detail, aggregated data from demographics/socioeconomics, and health systems.
Of particular importance are ‘high-resolution’ individual data to bridge the gap between simple description and the effective interpretation and public health use of cancer data (high-resolution studies have originated from the Eurocare database, where sampling of patients with more detailed clinical information has been carried out, and there is now a range of such studies in the Era-Net Transcan-2 Highcare project, and also in Rarecare, on rare cancers).
□ Prevention – fruit and vegetable consumption, smoking, body mass index, physical activity, alcohol consumption, sun exposure (from sources such as the European Health Interview Survey, EHIS, plus new ones on sun exposure for example)
□ Screening – mammography, pap smear, colorectal (EHIS and official member state reports)
□ Treatment and clinical aspects – radiotherapy equipment, CT/PET/MRI scanners, surgical procedures (hysterectomy, prostatectomy, breast conserving/ mastectomy etc.), stage, compliance with guidelines, treatment delay (from Eurostat, OECD, Eurochip plus new sources on staging, guidelines and delays)
□ Macro social and economic variables – health expenditure as % of GDP, anti-tobacco regulation, cancer patient costs (Eurostat, WHO; cost would be a new one)
□ Epidemiology and cancer registration – registry coverage, incidence, survival, prevalence, mortality (IARC, Globocan/ECO, Eurocare, Haemacare, Rarecare, Europreval, Eurostat)
See also the European Network of Cancer Registries – www.encr.eu and the European Cancer Observatory – www.eco.iarc.fr, for details on ‘precursor’ projects. www.tumori.net/eurochip has details on the now concluded cancer health indicator project.
Can we trust the data?
The Eurocare team, based at the National Cancer Institute in Milan and at the Italian National Public Health Institute in Rome, do discuss the limitations – and strengths – of their studies at length in their publications, so there should be no confusion about the interpretation of the findings. In the summary of results for Eurocare-5, they flag up a number of issues. These include the “unexpectedly high” survival rates some countries show for cancer types that are rapidly fatal; variations in case mix for cancers in the same main type (such as small-cell vs non-small-cell lung cancers); the well-recognised problem of the impact of screening in raising incidence and survival rates through overdiagnosis and lead-time bias in prostate, breast and melanoma in particular; and bias introduced by data that comes from cancer registries predominantly in affluent areas of a country (Italy and Belgium are mentioned).
But the key limitation is a big one – that there are no data on major prognostic factors such as stage at diagnosis and treatments. Without these it is not possible to fully assess the reasons behind survival differences, they report. At present, these data are available only on an ad hoc basis, as cancer registries do not systematically collect such clinical data and, even if they did, cancer staging practices vary across the continent, which would be another barrier (in Eurocare-5, of the 116 participating cancer registries, 43 did provide stage data for breast cancer but only 12 for prostate, for example).
Another shortcoming inherent in survival studies of this sort is that Eurocare is a retrospective study that records the five-year relative survival rates for patients diagnosed up to 14 years earlier. The current analysis, published in 2013, covers the period 1999 to 2007, and a lot can happen in healthcare systems and cancer guidelines between then and publication. (Eurocare-6, though, will analyse the prognosis for patients with a diagnosis between 2005 and 2012 with a follow-up to 2013, reducing the gap between data collected from registration time and published data.)
As for strengths, Eurocare-5 goes some way to addressing a major criticism of previous versions – lack of coverage. “National registries of Bulgaria, Estonia, Latvia, Lithuania, and Slovakia are now included,” write the team, “and population coverage also increased for other countries: from 1% to 23% for Germany, 34% to 100% for Netherlands, 8% to 100% for Czech Republic, 43% to 77% for Portugal, and 27% to 36% for Italy.”
And looking back at Eurocare-4, published in 2007, some of the criticisms levelled at the time of publication seem unfounded, in particular on the quality of the data and the lack of coverage.
The increased coverage now in countries such as Germany has not changed their survival ranking; indeed, the Czech Republic, which upped its population contribution to 100% in Eurocare-5, showed increased survival, not less, as might have been expected for a whole-country sample.
The Eurocare team also take pains to explain the rigorous quality control procedures they apply to the datasets. They point out that, even if one were to assume there is a high number of errors in cancer registries, this would still not explain the differences between the UK and other comparable European countries (there is a simulation study on this).
It is natural for oncologists to defend their practices and outcomes, and certainly there are many questions that can still be asked about the applicability of the data. But in the UK, the finding of Eurocare-5 that the country is still lagging behind its western European peers, albeit with a narrowing gap in some cancers, has been broadly accepted.
Finding out more
The issue now is to find out why and take steps to improve the situation. The key, for many, will lie in ‘drilling deeper’ to get a clearer picture of certain aspects of services and outcomes.
The Eurocare authors talk broadly about the possible explanations for differences between countries, which they say include “differences in stage at diagnosis and accessibility to good care, different diagnostic intensity and screening approaches, and differences in cancer biology”. Variations in socioeconomic factors, lifestyle, and general health between populations might also have a role, they add.
They also mention analyses that have been done in the UK to try to explain its relatively poor performance – in particular the role of late diagnosis (which is also a possible factor in Denmark, not least in lung cancer). Unequal access to and underuse of treatments have also been mentioned as contributory factors – older women in England, for instance, have been reported as having more non-standard treatments than younger patients.
For Richard Sullivan, director of the Institute of Cancer Policy at King’s College, London, the answers are to be found in joined up thinking about data and processes. “Epidemiological data is vital – you need mortality, survival, prevalence and incidence to tell you different things about your health system. But we have to drill down deeper to understand the differences, such as by adjusting for the stages of cancer that people present with.
“The countries making the most progress, such as the Netherlands, are the ones able to use the data to develop quality systems and processes for the delivery of care, down to factors such as the volume of surgery needed at a centre, the amount of radiation fractions to provide and so on.”
This also depends on policymakers gathering the data and understanding how healthcare systems should be organised and prioritised to provide cancer services, he adds. Much of this goes by the board in less regulated countries, particularly in eastern Europe. “Because of the lack of outcome data, people are able to claim what they want without being held to account. A big problem is that epidemiological systems are often poorly funded – registries are just not as sexy as other things such as drugs,” says Sullivan.
A number of countries, such as Greece, do not yet have national population cancer registries, or indeed properly implemented cancer plans, and while it is possible to model data across regions and population groups – Eurocare divides its datasets into regions – the type of high-level intelligence that also involves the regulatory and economic issues needed to plan and implement cancer services is often lacking and not prioritised, he adds.
Where’s the UK going wrong?
The UK, meanwhile, has different health systems in its four constituent countries, and although much work has gone into developing tumour-based clinical pathways and other processes, most cancer services are carried out in general hospitals, and systems are subject to constant reorganisation and changes in commissioning policy, according to fiscal cycles, notes Sullivan.
The latest cancer taskforce report for England – Achieving World-Class Cancer Outcomes – which sets out a strategy up to 2020, once again uses international comparisons, noting that the gap in survival between the highest performing comparable countries (Australia, Canada and Sweden) and the lowest (England, Northern Ireland, Wales and Denmark) remains largely unchanged, except in breast cancer.
“Commissioners consistently report they have neither the expertise
nor the time adequately to commission complex cancer services”
It recognises the higher incidence of cancer in deprived groups, but argues that differences in one-year survival among England’s clinical commissioning groups cannot be explained only by deprivation levels (although certain factors can be critical, such as the higher incidence of triple negative breast cancer in African–American women). The report also references Eurocare-5 in noting that treatments have become more important in accounting for international differences.
But commissioning of cancer services has become highly fragmented, and the strategy taskforce claims that commissioners “consistently report they have neither the expertise nor the time adequately to commission complex cancer services, many of which are changing rapidly as research drives progress.” Fragmentation of services is also cited as a problem by the head of the Danish Cancer Society.
The English taskforce comes up with a number of expected recommendations, such as retargeting early diagnosis efforts, replacing outdated radiotherapy equipment, and rolling out a national molecular diagnostic service. But possibly one of the most interesting proposals is to provide better metrics that give more rapid feedback through a ‘dashboard’ that will include regularly updated data on the vital statistics of a service, which could help address complexity.
For Sullivan, this is fine, but he argues that reports like this one are too often written by insiders rather than external experts, and there is resistance to taking the hard decisions to act on data. He gives as an example research carried out by Henrik Møller’s group at King’s College, which found that hospitals in England that carry out high volumes of surgery for non-small-cell lung cancer have more patients who are older, of lower socioeconomic status and have more comorbidities – and yet achieve better survival. “But despite this we seem to be unable to consolidate thoracic services in England,” says Sullivan.
International comparative studies provide important indicators
to drill down into to try to discover reasons
This is the type of study that interests Lars Holmberg, a breast cancer surgeon turned cancer epidemiologist, who also worked at King’s but is now back home in Sweden at the Uppsala/Örebro regional cancer centre. Holmberg has led epidemiological studies such as a comparison of prostate cancer survival in England, Norway and Sweden (Cancer Epidemiol 2012, 36:e7–e12). His view of the international comparative studies is that they do have major limitations, and “making far-reaching conclusions from them is a mistake”. They do, however, provide important indicators to drill down into to try to discover reasons. “And maybe it’s not that useful to keep on doing these broad comparative studies – perhaps we should ask more specific questions about possible interventions,” he suggests.
Drilling down for explanatory data
Survival data indicate that older women in the UK have poorer survival than their peer group in neighbouring countries. Drilling down to look at treatment data reveals that the poorer survival could be because in the UK they are less likely to be treated according to guidelines. Drilling down further, to look at the use of geriatric assessment, could reveal whether they are being undertreated because of unwarranted assumptions about their fitness, or whether this generation of women really is more frail in the UK than in neighbouring countries, in which case less aggressive treatment could make sense.
Holmberg points out that attempts to improve the data by which to compare countries, such as adding the stage at diagnosis, may not be very productive, as clinical variation may be great, even if the quality of the data is fine. And patients in one country who present late may get better treatment than in another country, which could confound comparisons.
During his time in the UK, Holmberg recognised that later diagnosis, especially in cancers that are curative when caught early, is one explanation for the country’s poorer outcomes. He also echoes other commentators in flagging up undertreatment of older patients as a possible contributory factor. “When comparing England and Sweden, England appears to recommend active treatments for older people less frequently, although that may have changed now,” he says. He cautions, however, that lower rates of active treatment could be appropriate if older people in England have more comorbidities, in which case, he says, “it wouldn’t be reasonable to put them through the stress of treatment.”
Holmberg suggests that a study on geriatric specialists assessing older people for treatment would be a good example of research that is worth performing across a select group of countries. “What I’ve seen in epidemiology is that pure data gathering is often over-emphasised, and hypothesis testing under-emphasised,” he says.
Even Sweden needs to drill down…
Sweden has good data, through mandatory cancer registration and clinical audit of hospitals, and is among the top-performing countries for cancer. But even here, clear differences in outcomes are apparent between regions and between socioeconomic groups, says Holmberg. It is the deeper study designs that are needed to root out the causes, he argues, mentioning a prostate cancer clinical database project in Sweden, PCBaSe, which found, for instance, that the diagnostic assessment of patients can differ by socioeconomic status. “Higher status men get a more thorough work-up,” he says. Again, this could be the basis for a cross-country study.
“It doesn’t help to have a high-volume hospital if processes are disorganised.”
A similar story has been reported for breast cancer, where Swedish counties with less good results have been found to differ from others, again through the intensity of diagnostic work-up. “Maybe the women with less good outcomes got the right treatment based on what the oncologist knew, but maybe the information was wrong,” says Holmberg. Was socioeconomic status a factor? It is a question worth answering, he feels.
The extent and quality of multidisciplinary working is another factor suggested by Holmberg as a possibility for investigation. “My view is we tend to look at surgeons and their volume of work, but we have neglected to look more deeply at teamwork, all the way from diagnosis to follow-up. It doesn’t help to have a high-volume hospital if processes are disorganised.”
The Eurocare team adds that studies on process, such as organisation of care, are indeed important, and also mentions survivorship and quality of life research, and outcome research, which identifies short-term outcomes as surrogate endpoints of survival. But they stress that large-scale comparisons remain important to study the overall impact on survival over time and regions.
Putting data to work
Someone who is well-placed to pull much of this discussion together is Alexander Katalinic, director of the Institute of Cancer Epidemiology at the University of Lübeck, Germany. He is in charge of the regional cancer registry (Schleswig–Holstein), chair of the Association of Population-Based Cancer Registries in Germany, chair of the steering committee of the European Network of Cancer Registries (ENCR), member of the Eurocare steering committee and, not least, one of the team behind the nascent European Cancer Information System (ECIS).
Benchmarking means learning from the best in an atmosphere of trust
– no one, especially the hospital managements, wants to see
their clinic’s data exposed as poor in the newspapers.
He confirms that Eurocare has been important for Germany, especially in stimulating the setting up of registries that now cover the whole country, as well as a 2013 law that compels all regions to collect more clinical data to do more quality assurance. Speaking about the Schleswig–Holstein registry, Katalinic says it has complete data for the region.
“And we really use the data – it isn’t a graveyard as some are,” he says. “We have good contacts with the clinicians in the region, and of course they want good results for their patients, and the registry enables them to discuss the quality of their clinics. Benchmarking means learning from the best in an atmosphere of trust – no one, especially the hospital managements, wants to see their clinic’s data exposed as poor in the newspapers.”
As a cross-border example, Schleswig–Holstein ran a project with neighbouring Denmark comparing lung cancer survival. It found that those Danish patients who survived more than six months had the same survival as patients in the German region, which could prompt hypothesis-driven research into possible socioeconomic, comorbidity and other factors that Holmberg advocates.
Katalinic though is much more bullish about the potential for large-scale comparative data as a policy tool. The ECIS has grown out of various European projects including Eurocare, Eurocourse (on the development of population-based cancer registries), the Eurochip cancer health indicators initiative, and in particular the information and data work package of the European Partnership for Action Against Cancer, led by Milena Sant of the Eurocare team at Milan’s Istituto Nazionale dei Tumori.
It aims to provide a single interactive platform for exploring comparative data, by country, age, gender and time point, on incidence, mortality, prevalence and survival, together with a range of additional cancer health and system indicators (see box on top). Importantly, says Katalinic, it will be set up to be sustainable, with a project team at the European Commission’s Joint Research Centre in Italy committed to its development. There is much to do on data analysis and quality, and the project should also highlight ‘white spots’ around Europe where there is no or limited registry data.
One of the first tasks of the new information system will be to publish data on cancer incidence, which Katalinic says can translate into public health action. “Countries can benchmark incidence in the same way as we are doing survival – take colorectal cancer, where, if you monitor where screening is in place, you can now see clearly where incidence is falling.”
One of the aims, he says, is to create an interactive tool, similar to Nordcan, which is already up and running for the Nordic region, hosted by the International Agency for Research on Cancer, IARC.
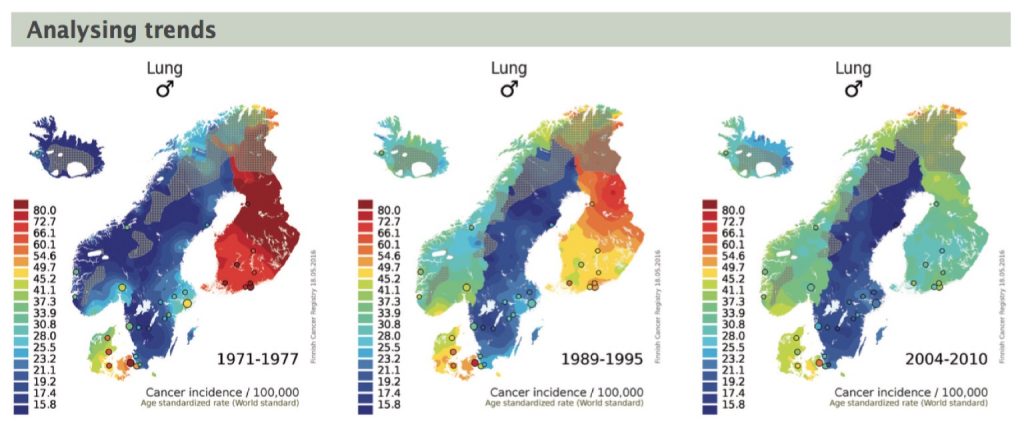
One such tool enables users to see comparative trends in incidence and mortality, through an animated colour-coded map, operated by a digital slider that moves from one time period to the next. The information can throw light, for instance, on how lung cancer incidence has responded to anti-smoking policies, says Katalinic.
In the longer term, the key aim for ECIS is to make available individual-level data, like the US SEER – Surveillance, Epidemiology and End Results – programme, which researchers can draw on for high-resolution studies to explore the impact, for instance, of compliance with guidelines on survival or mastectomy rates.
Key to it all will be ensuring high-quality data, says Katalinic, who adds that, despite reservations by some, it is possible to collect more clinical data such as tumour stage that will be amenable to comparative analysis.
Indeed, a new data protocol for European epidemiological cancer studies has already been defined, which envisages the collection of standard data on stage at diagnosis and summary treatments, so that over the next few years, incidence and survival by these factors will be available for research (see ENCR’s data call 2015).
What can data do?
Will this give countries like the UK and Denmark – or indeed countries that rank even lower – the information they need to address the problems that dog their cancer systems? The indications so far would suggest probably not.
Given the complex interactions where social inequality and differential access to resources may be overriding factors, it is unlikely that focusing on individual disparities, for instance in late diagnosis, or access to new drugs, or hospital systems, will make a big difference. Indeed, the Eurocare team stresses that interventions that address the whole system, rather than measures for selected groups of patients, are likely to make the most impact on survival. But in the future, ECIS data could be essential to generating hypotheses that could be tested in the sorts of studies advocated by experts like Lars Holmberg.
It could also provide an invaluable audit service. As well assisting policy makers in teasing out the implications of five-yearly reports of survival data, it will aim to provide other comparative information on a range of quality indicators that are not routinely collected by cancer registries, and which could be available much sooner, so that problems can be picked up quickly and the impact of remedial actions on those indicators can be monitored effectively.
But health policymakers across Europe do need to support cancer registries in collecting more basic clinical data to pave the way for a wider indicator set.





