With the prospect of a chemo-free cure for some blood cancers, and with new targets and new drugs emerging at an unprecedented pace, Simon Crompton asks: Is haematology where the promise of precision medicine will finally be realised?
We have come a long way since pioneering French microscopist Alfred Donné provided the first cellular description of a blood cancer in 1844. “More than half of the cells were mucous globules [white cells],” he wrote, which “dominates so much that one wonders, knowing nothing about the clinical course, whether this blood does not contain pus.”
In the past 60 years, haematological cancers have provided the testing ground for systemic therapies, the first cure by chemotherapy, the first proof of principle of targeted medicines.
In the 1960s, the first chemotherapy cancer cure came with MOPP (nitrogen mustard, oncovin, procarbazine, prednisone) for Hodgkin lymphoma. In the late 1990s, rituximab for non-Hodgkin lymphoma was the first monoclonal antibody to be approved by the US regulators. And imatinib, the first anti-cancer tyrosine kinase inhibitor, was approved for chronic myeloid leukaemia in 2001 – and has since dramatically improved the outlook for the disease in the solid gastrointestinal tumour GIST.
“Over the past 65 years, survival rates for many blood cancer patients have doubled, tripled and even quadrupled,” says Louis DeGennaro, CEO of the Leukemia and Lymphoma Society. “Almost 40% of the new cancer drugs developed since 2000 were first approved for blood cancer patients, and are now helping patients with other cancers and chronic diseases.”
The figures tell the story of how innovation in blood cancer continues. The FDA has designated 12 novel blood cancer therapies as “breakthrough medicines” – requiring expedited development because of their promise in treating a life-threatening disease. Around 250 of more than 800 cancer medicines in development are in leukaemia, lymphoma and multiple myeloma. And genetics studies have recently revealed there are at least 35 types of leukaemia and 50 types of lymphoma – each with distinctive characteristics to target.
“There are multiple advances happening at the same time, reflecting an explosion of knowledge in haematological cancers,” comments Anas Younes, medical oncologist and head of the Lymphoma Service at Memorial Sloan Kettering Cancer Center in New York. “It sounds like a cliché but it’s true.” Along with others working in haematological cancers, Younes believes there is now the genuine prospect that, as precision medicines become more widely embedded into clinical practice, the days of toxic chemotherapy may be numbered. At least in blood cancers.
Given the continuing frustration over the unfulfilled promise of precision medicine in solid tumours, the question then arises: Would the rest of the cancer world do well to pay more attention to the new paradigms that are proving their value in many blood cancers?
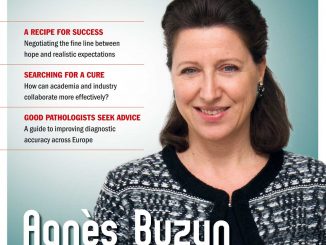
Franco Cavalli, Scientific Director of the Institute of Oncology of Southern Switzerland, believes they would. He argues that the difficulties for precision medicine stem mainly from the heterogeneity of the tumours – a challenge which he says was first encountered in blood cancers. “Now, the experience in blood cancers of efforts to overcome such difficulties – for example, devising groups of patients who are as homogeneous as possible – may serve as a guide for many solid tumours as well.”
In his editorial in this issue, he points to the increasing separation of haematological and solid tumours in the training of medical oncologists, and argues that specialists in solid tumours could glean valuable insights into the basics of tumour biology by paying more attention to developments in haematological oncology.
Hodgkin lymphoma and the quest to end toxic treatment
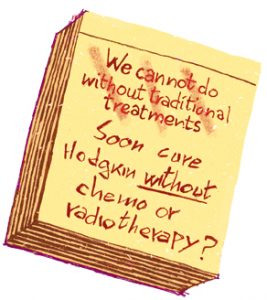
The benefits of moving from chemotherapy-based regimens to ones based on precision medicine are amply demonstrated in Hodgkin lymphoma. Although aggressive chemotherapy and radiotherapy regimens made Hodgkin lymphoma one of the first curable cancers in the 1960s and 70s, the cost was high.
Studies indicated that the risk of developing neoplasms after treatment was 18 times higher than in the general population, and people who survived Hodgkin (which most commonly affects young adults) were at increased risk of coronary artery disease, valve disease, congestive heart failure, pericardial disease, stroke, arrhythmia and sudden cardiac death.
The advent of the monoclonal antibody drug brentuximab vedotin five years ago brought a radical change, bringing induced remission in 75% of patients with relapsed or refractory Hodgkin. Today, according to Andreas Engert, professor of internal medicine, haematology and oncology at the University Hospital of Cologne, new data will show that the drug works well as a first- and second-line treatment in combination with chemotherapy.
“But in the end, brentuximab vedotin is still a kind of targeted chemotherapy, and patients who have received a lot of chemo are more likely not to respond to brentuximab. That could be a problem for heavily pretreated patients.”
New immunotherapy approaches provide the promise to solve the problem. The first immune checkpoint inhibitor in lymphoma, nivolumab, was approved by the FDA for relapsed or refractory classical Hodgkin lymphoma in May 2016. It is the first monoclonal antibody targeting the programmed death-1 (PD-1) immune checkpoint pathway. The effect is to enhance T-cell anti-cancer activity and induce tumour cell disintegration.
Early phase trials indicated a good safety profile, and 66% of patients achieved an objective response after nine months (assessed using immune-related response criteria – IrRC). New trials presented this year at ASCO indicated an objective response rate of 65% after 19 months in patients who had previously had autologous stem cell transplants (ASCT) but not been treated with brentuximab vedotin. There was a complete response in 29% of patients. Engert’s centre in Cologne became involved in the trials at an early stage – having “banged on the door” of Bristol-Myers Squibb to expand the trial from the United States to Europe.
“We are using these antibodies right now in the relapsed and refractory setting,” he says. “We saw many patients who we originally thought might be too frail, who responded remarkably well.”
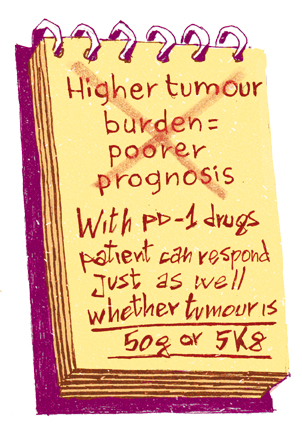
The drug, he says, has completely changed expectations about response and cure. “It doesn’t matter if the patient has a 50 g tumour or a 5 kg tumour – the patient can respond just as well with PD-1 drugs. That’s remarkable, and it completely interferes with our knowledge about who’s going to respond and their chances of cure.”
The latest nivolumab trial results, announced at ASCO in June and then presented by Engert at the European Hematology Association Congress in Madrid, demonstrated responses in adults with relapsed or progressed Hodgkin lymphoma after ASCT, irrespective of whether they had also been treated with brentuximab vedotin (BV). In the group that had BV therapy after ASCT, the objective response rate was 68% after 23 months, with complete response in 13% of patients.
“The new data look great,” says Engert. “In particular, it is quite astonishing to see that those patients who just achieved a partial response or stable disease still did remarkably well overall. This is a clear indicator that PD-1 inhibition offers a really new and different mechanism of action.
“It’s very surprising and rewarding to see these major achievements. Now there’s a good chance of curing patients in both the early and advanced stages of the disease. That’s particularly good news for young patients with Hodgkins.
“The development of these new antibodies is exciting because it will reduce long-term side effects in young people. We’re conducting studies in early stage patients and I’m convinced it will take just a few more years before we can say with conviction that we can cure Hodgkin patients without chemotherapy or radiotherapy. I think that’s what we always wanted to achieve.”
However, there is a problem in bringing these advances to fruition. Drug companies, says Engert, are reluctant to invest in Hodgkin trials because they are overwhelmed by opportunities in solid tumours. “It’s a question of where you put your money, and where the highest value is. So far we have done well with brentuximab and the PD-1s. Some companies are uncertain if they want to invest in first-line Hodgkin treatments with much bigger trials, but I think data is going to look so good that they will have to.”
Targeting the micro-environment: learning from CLL
The story of chronic lymphocytic leukaemia (CLL) provides another example of how precision medicine paradigms are playing out in blood cancers.
 Twenty years ago, little was known about CLL, which accounts for around a third of all leukaemias worldwide. We knew that it affected the B-cell lymphocytes. We knew there were two types, determined by the presence of mutations in the immunoglobulin genes – one aggressive and requiring treatment, one more indolent. We knew that the leukaemia carried a few recurrent cytogenetic abnormalities, but how they contributed to the disease was unclear. We knew that the treatment invariably revolved around chemotherapy – sometimes combined with a monoclonal antibody (chemo-immunotherapy). And we knew that it was incurable.
Twenty years ago, little was known about CLL, which accounts for around a third of all leukaemias worldwide. We knew that it affected the B-cell lymphocytes. We knew there were two types, determined by the presence of mutations in the immunoglobulin genes – one aggressive and requiring treatment, one more indolent. We knew that the leukaemia carried a few recurrent cytogenetic abnormalities, but how they contributed to the disease was unclear. We knew that the treatment invariably revolved around chemotherapy – sometimes combined with a monoclonal antibody (chemo-immunotherapy). And we knew that it was incurable.
“When we had only chemo-immunotherapy, there was a proportion of patients that was chemo-refractory – and this proportion was larger the more the disease was treated,” says Davide Rossi, leader of the experimental haematology group at the Institute of Oncology Research, Switzerland. “We were unable to provide effective treatment for these patients.”
Chemo-immunotherapy failed in 20–25% of patients. For these patients with ultra-high risk CLL, survival after failure was less than three years, and the only effective salvage option was an allogeneic stem cell transplant. The rigours of this approach, however, meant it was only available to a minority of patients who were fit or young enough.
Then, three years ago, everything changed, with the introduction of two new types of compound – one that inhibits the signalling between the cancer and its micro-environment, and one that blocks the signalling that prevents cell death. The drugs are: B-cell receptor (BCR) inhibitors, such as ibrutinib and idelalisib, and B-cell lymphoma 2 (BCL-2) inhibitors, such as venetoclax.
Durable responses are now common in many patients with previously relapsed CLL. “In clinical practice, we now have potent drugs that almost, although not completely, overcome chemo-refractoriness in CLL,” says Rossi. “In ultra-high risk patients, ibrutinib, idelalisib and venetoclax all provide an unprecedented high response rate in the range of 70–80%, which are durable.”
This, he said, points the way towards the end of what he calls “bombastic” therapy – the old paradigm of bombarding the patient with treatments. Clinical research is now investigating the possibility of combining BCR and BCL-2 inhibitor drugs with each other, and also with other monoclonal antibodies, “to try to provide deep responses and hopefully the cure for CLL”.
The significance of the CLL revolution goes beyond a single disease. Rossi says it is exciting because it demonstrates the absolute dependence of many cancers on their microenvironment – and ways to exploit that weakness.
“There’s a long story of basic and translational research in CLL that, in the end, established the addiction of this tumour to signals coming from the microenvironment, to gain survival and proliferation signals,” says Rossi. “Many cancers are addicted in the same way. The key point is understanding which of the cellular programmes and pathways are central, and are to be targeted. In CLL, we gain this understanding from fundamental science.”
“I want to underscore that CLL is a paradigm, because as well as BCR inhibitors, which interfere with the mechanisms coming from the microenvironment, we have the BCL-2 inhibitors, which block the anti-apoptotic cellular programmes, which tumours activate through genetic lesions. So we are addressing both the microenvironment and the genetics of the tumour as drivers of cancer.”
Nearing a chemo-free cure
The move towards precision medicine in CLL could herald the end of chemotherapy for many patients, says Rossi. A BCR inhibitor has already been approved as a first-line monotherapy for CLL patients in the United States and Europe. And there are hopes that, within three years, the results of trials combining different BCR and BCL-2 inhibitors may indicate that combinations bring longer remissions, and reduce the need for long-term treatment.
The prospect of chemo-free treatment spreads far beyond CLL. A multiple myeloma diagnosis used to mean a life expectancy of three to five years, with standard treatment consisting of chemotherapy and stem cell transplant. Today, average survival has nearly trebled thanks to new proteasome inhibitors, immune-modulating therapies like thalidomide – and then combinations of these drugs with steroids, in doublet and then triplet therapies.
A randomised trial presented at the American Society of Hematology last year suggested that triplets should now be the standard of care for patients newly diagnosed with multiple myeloma.
“Today, we have learned to talk in terms of tablet triplets,” says Rossi. “In the future, I can see the possibility of a chemo-free, novel agent based treatment paradigm for every CLL patient.”
Philippe Moreau from the University Hospital of Nantes, France, believes that for the first time there is the possibility of curing the 50–70% of multiple myeloma patients who are classified as “standard risk”, using all the effective drugs and stem cell treatments. “The goal is to achieve very fast and very deep responses and to reach minimal residual disease negativity,” he says.
The challenge of exponential knowledge growth
But the explosion of knowledge in blood cancers also presents massive challenges. Researchers and clinicians have at their fingertips exponentially increasing data about their genetics, subtypes and precise biological relationship to their microenvironment. Dozens of novel therapies are being developed, each of which may have a more potent effect if used in combination with any of dozens more.
Yet there are only limited clinicians, researchers and facilities to be able to act on the information. So where do priorities lie?
Franco Cavalli believes that increasing knowledge about different molecular types of blood cancer requires a rethink about how resources are allocated.
“What were once a handful of haematological cancers are in fact hundreds of different ones when you look at their molecular biology. So this re-classifying has implications for specialist pathology and for specialisation.
“Classifying individual cancers has become very difficult, so worldwide the big problem is how to have a correct diagnosis. And haemato-oncologists may also now have to subspecialise. There are already specialists in leukaemia, lymphoma and myeloma. This is making everything more expensive and more difficult in terms of practical organisation.”
According to Anas Younes, who conducts translational research into novel treatment strategies for Hodgkin and non-Hodgkin lymphoma at his own laboratory at Memorial Sloan Kettering, the key to moving forward constructively is to rationalise. For example, all the new molecular information characterising different types of cancers needs to be reviewed – and the cancers need to be re-categorised into types that are clinically useful, not simply observable.
“The trend is divide and conquer,” he said, “slicing each large cancer type into small pieces.” But classifying them according to morphology, clinical behaviour and genetic composition is not in itself useful. “We need to slice them based on a genetic landscape that is actionable – not just saying a particular biomarker expresses so and so. Unless it’s actionable it’s not going to help me design a clinical trial.
“So at Memorial, we’re going backwards to try and re-group lymphomas into common baskets that share actionable genetic alterations or activated oncogenetic pathways – then try to build clinical trials based on that. So there’s a huge effort going on trying to authoritatively gene sequence all the different types of lymphoma.
“Every patient who walks through our doors is asked to fill out a consent form, and we will sequence their tumours for free, to collect this information. Then we can decide which genetic alterations are common across different subtypes, and then design clinical trials based on that.”
There is no doubt that dividing diseases like CLL into subtypes according to biomarkers is very useful, says Davide Rossi. For example, in CLL the mutational status of the immunoglobulin gene provides prognostic information as well as informing therapy. And the status of the p53 gene can stratify patients according to which will respond best to chemo-immunotherapy.
“But perhaps in the future it may not be the same,” says Rossi. “Now the field is quite confused because we don’t have a lot of clinical studies to support our treatment decisions, so we have to support them by biomarkers. But in the future, who knows? Will we still need biomarkers, if treatments become chemotherapy free? It’s a field in continuous evolution.”
The challenge of prioritisation
For Anas Younes, the single most important challenge as knowledge explodes in blood cancers – and increasingly in all cancers – is how to prioritise the research agenda.
“We now have more than 600 agents available in pre-clinical testing or testing for cancer, he says, “and we never had this before. So how do you choose? Every time you commit yourself to one trial you’re locking in your patients, your progress, your resources for at least three years. You can’t test all of them at the same time.”
The problem escalates, because combinations need to be tested. Very few cancers have one unique Achilles heel – most use multiple oncogenetic pathways to thrive. So finding drug combinations to inhibit several pathways simultaneously is essential. Younes points out that a vital next step is to test immune checkpoint inhibitors in combination with other immune therapeutic agents, small molecule drugs or even traditional chemotherapy. But trialling just ten drugs in all their doublet combinations could take 90 years. “So how do you prioritise those combinations?”
The answer, said Younes, is to use preclinical studies to try to establish the most promising drugs and combinations – evaluating safety and then comparing them head to head. These preclinical studies need to be run completely independently of drug companies.
“You need to step backwards and be an independent judge, because each sponsor comes to you with their own ideas, but it might not be the best idea. So it’s very important for academic centres to do these combinations in an unbiased way – test in vitro, and then in mice. Then, even if two combinations seem to meet in efficacy, you can see which has the best safety profile and make a judgement as to the best available based on your own data.”
“It’s not perfect. But that’s what larger cancer centres are doing these days – they’re no longer being passive recipients from sponsors who ask you to do things.”
Setting an agenda
No one, says Younes, could claim that developments in blood cancer are ahead of those in solid tumours. “There are areas where blood cancer is leading the way and other areas where we’re learning from solid tumours. The reason is that a lot of knowledge is being shared, and this is because there are shared genetic alterations among some solid tumours and some blood cancers that can be targeted.
One area he mentions where blood cancers are “way ahead” is in developing chimeric antigen receptor (CAR) T-cell therapies – a novel type of immunotherapy which early trials have shown to be effective in patients with refractory lymphoma and leukaemia (see box).
But as he adds, “Just for practical reasons, some solid tumours that have a high frequency and a higher unmet medical need – like lung, colon, breast and prostate cancer – tend to have more funding and concentrated clinical research effort, so they often take an early lead.”
The fact is that the most common cancers will always attract the big research investment. But given their annexed existence from the mainstream of funding, discussion and research focus, haematological cancers are still charting a remarkable course in unlocking the potential of precision medicine. The way in which clinicians, researchers and funders build on the explosion of knowledge in the next ten years will demand the attention of the rest of the cancer world.
Learning from blood cancers: CAR T-cell therapy
Chimeric antigen receptor T-cell therapy is an experimental form of immunotherapy that revolves around genetically engineering T-cells to recognise and then attack cancer cells.
Groundbreaking studies have shown durable complete remissions in patients with therapy-refractory lymphoma and leukaemia. The results prompted the US regulators to grant CAR T-cell therapy breakthrough status for B-cell malignancies like acute lymphoblastic leukaemia and chronic lymphocytic leukaemia, as well as B-cell lymphoma and non-Hodgkin lymphoma.
“This is a rapidly growing field,” says Anas Younes, head of the lymphoma service at New York’s Memorial Sloan Kettering hospital, “but I think CAR T-cell therapy in liquid tumours is way ahead of solid tumours. The platform technology is now beginning to be applied in solid tumours.”
There are now more than 100 CAR T-cell clinical trials running. In November 2016, Novartis presented results from a phase II trial with its CAR T-cell therapy CTL019 for B-cell acute lymphoblastic leukaemia. It achieved remission in 82% of patients after three months. This is in a disease with limited treatment options, where currently the chance of survival for children who relapse or fail to attain remission is between 16% and 30%.
The company is preparing to submit applications to the FDA and EMA this year.
Severe side effects, which have included deaths in early trials, are a problem with CAR T-cell therapy. Cost is also an issue. The EMA believes “there are still scientific and regulatory challenges to overcome to bring these innovative products to the market.”