In 2006, Slovenia staged the ‘United Against Cancer’ summit, with a view to closing the gap in prevention and survival between ‘old’ and ‘new’ Europe. Tit Albreht, from the National Institute of Public Health, was a key player. He went on to pioneer a series of EU Joint Actions on cancer, where member states collaborated on approaches to planning and implementing patient-centred integrated cancer services. Cancer World asked him why he did it, what the impact has been, and what should happen next?
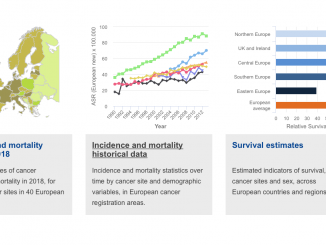
Cancer World: The 2006 ‘United Against Cancer’ summit in Ljubljana took place in the context of a ‘new Europe’, with EUROCARE data revealing a large survival gap between old and new member states. What were you hoping to achieve?
Tit Albreht:
 Central and eastern European (CEE) countries were not happy about lagging behind western Europe. The idea behind that conference was to highlight the possible reasons for that survival gap. At that time people tended to assume the reasons were purely financial: western countries have more to spend on sophisticated expensive technologies that we cannot afford, so we are condemned to lag behind. By that logic, the only option was to focus attention on prevention, health promotion, and maybe also screening programmes for early detection. But cancer is a unique and complicated disease, and we wanted to highlight the importance of all the disciplines, all the professions, and all the topics that need to be covered – not only epidemiology, or diagnosis, but also treatment, palliative care, survivorship, rehabilitation, research, and strengthening the registries.
Central and eastern European (CEE) countries were not happy about lagging behind western Europe. The idea behind that conference was to highlight the possible reasons for that survival gap. At that time people tended to assume the reasons were purely financial: western countries have more to spend on sophisticated expensive technologies that we cannot afford, so we are condemned to lag behind. By that logic, the only option was to focus attention on prevention, health promotion, and maybe also screening programmes for early detection. But cancer is a unique and complicated disease, and we wanted to highlight the importance of all the disciplines, all the professions, and all the topics that need to be covered – not only epidemiology, or diagnosis, but also treatment, palliative care, survivorship, rehabilitation, research, and strengthening the registries.
Even when it came to screening, which many CEE countries were very enthusiastic about, the policy focus tended to be on the technology: we will buy machines, mammograms, laboratory equipment and everything will be sorted out. So we addressed this topic in the first Joint Action, which, in addition to developing recommendations on national cancer plans, also drew up guideliens on how to set up quality assurance systems to make sure the training, quality control, and structures are in place to make the programme work well.
CW: Healthcare is done very differently across Europe. Can policy on cancer services developed at a European level affect what health services actually do?
TA: The approaches and methodologies are often more important than how they are carried out. Take the example of multidisciplinary teams. MDTs are a necessity nowadays. It cannot be only the surgeon, or the first doctor to see the patient, who decides that patient’s fate. But even if everybody is convinced of the need to work in MDTs, it can be difficult to do if the policy makers don’t understand what they must do to make it happen. I was in Serbia recently, where people told me they are expected to spend up to four or five hours in MDT meetings that are held in the evening and are unpaid, because it is not recognised as work. This doesn’t make sense in a country where human resources are relatively cheap – at least compared to the cost of technologies, where poor countries pay the same as richer ones. And this is not limited to Serbia. There are still many countries where the key decision remains with the surgeon alone.
Then there are the broader questions about what is involved in delivering care along the whole pathway, starting with screening or early detection and ending with palliative care or rehabilitation or some other intervention. For every step of this trajectory we need quality guidelines and we need to map needs and capacity to secure resources. Once we map it, we can say: we need more trained providers of supportive care, or psycho-oncological support and so on. That mapping approach applies everywhere, even if countries differ in the way they address those unmet needs.
CW: Countries don’t like being told how to run their healthcare. Were you able to overcome that resistance?
TA: The thing about Joint Actions is they are part funded by the EU but are led by member states, so they are not seen as ‘top down’. That helps, not just because of the current political concerns of many countries, but also because people from each country are involved in developing the recommendations or at least have that opportunity. It is also helpful not to feel constrained by having to produce a legal document or guidelines that would be seen as binding. It is a more open way of reaching consensus on topics of common interest.
CW: After the Joint Actions end in 2021, will that be the end of European collaboration on cancer services?
TA: After nine years, and a lot of work done, I would be really sorry if we cannot find a body to take some of this work forward. We are talking to the Commission about where we could make a repository and which topics could be kept alive. We need a structure, for instance, that can update and respond to the challenges in cancer screening. The EU recommended screening for colorectal cancer in 2003, more than 15 years ago, but so far only eight members states have fully put that in place. And now we have demands for new types of screening for cancers such as lung and prostate.
One possible body to take this forward would be the Joint Research Centre in Ispra, Italy, which is home to the European Network of Cancer Registries. They’ve also done a great job with the European Commission Initiative on Breast Cancer, and they are currently doing something similar for colorectal cancer.
CW: What role do you think ECCO, as Europe’s multidisciplinary cancer organisation, should play in taking forward the cancer care policy agenda?
TA: Everyone who has a clear idea of the changes they want to see should get involved. In that respect, I think ECCO has the right people and they know the issues. The problem is that this work needs proper funding. Everybody talks about policy, and everyone wants to influence policy, but nobody wants to finance this work. This is also our problem with the Joint Actions. When you call a meeting to discuss policy on a particular cancer issue, you will always have a large audience. But when you say “let’s work together on topics of common interest, but you will all have to input your efforts and energy and money for this to go further,” then you face a problem.
The reality across healthcare in general is that health systems research is insufficiently funded. You may get €500,000 for a project where you have to do a lot of work and surveys and so on, while people who do basic research will get €10 million. When the two types of research go hand in hand, as they do for example in the UK, it is possible to identify the gaps and issues that need to be addressed. But not all countries are equipped to do that research at different stages of the system. I think this is probably the most important challenge for the future.
Tit Albreht is Senior Health Services and Health Systems Researcher at the Slovenian National Institute of Public Health. He helped organise two European cancer conferences in 2006 and 2008, hosted by Slovenia. He led the National Cancer Plan work of the first Joint Action (EPAAC 2011-2014) and coordinated the CanCon Joint Action 2014-2017 and the current iPAAC Joint Action 2018- 2021. Recommendations from those European cancer policy collaborations were published in a series of e-books: