Little by little, patient advocates are winning their battle to be involved in decisions that affect them. They are now focusing on how to use their new-found voice to deliver real change for the people they represent.
The days when patient groups were all about tea and sympathy are long gone. Over the past 20 years or so, cancer patients who choose to become active have focused increasingly on advocacy: campaigning for greater public awareness, lobbying for improvements in patient care, and educating patients about their disease and treatment options so they can play an informed role in decisions about their own care. They have also been knocking on the doors of researchers, regulators and policy makers, demanding the right to have a say, as equal partners, in decisions that affect them.
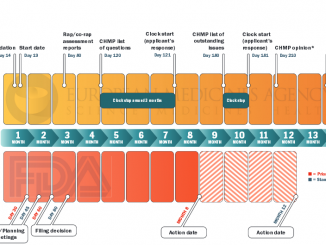
Slowly but surely, doors have started to open. Some national health technology assessment (HTA) bodies invite patient advocacy groups to submit evidence on the impact of new drugs and other ‘medical technologies’ on their quality of life. Some trial sponsors consult them over priorities and acceptable trial designs. Europe’s regulatory body, the European Medicines Agency, is beginning to involve patient advocates in the approvals process. Some funders even include patient group involvement as a criterion, or at least a plus point, when awarding research grants.
While progress is patchy, this seems to amount to a welcome trend towards the ideal of “nothing about us without us”, adopted as a motto by the European Cancer Patient Coalition (ECPC). But contributing at this level poses a huge challenge for patient advocacy groups, whose members work largely on a voluntary basis, with little or no background in medicine or in running an organisation at a national – let alone international – level. They have to tackle this role on top of the effects of living with cancer or the legacy of having gone through cancer, or having lost someone to the disease.
In May, advocates representing a wide range of cancer patient groups gathered in Baveno, Italy, for a Masterclass to help them fulfil the ‘expert partner’ role they have been demanding.
Valued as partners?
Sitting at a table alongside scientists, regulators, health economists or health technology assessors can be a scary business, and even the more experienced advocates admitted they sometimes feel intimidated. They shouldn’t, was the message from Ken Paterson, former chair of the Scottish Medicines Consortium, the body that evaluates new drugs for funding.
Patients bring to the table expertise that is both valuable and unique, Paterson said. While clinical trial data for a new drug focus on its ‘anti-cancer’ properties, what HTA bodies care about is its ‘pro-patient’ properties – and there is often no direct correlation. Only patients can say how their disease impacts on them and on their families. “They know the problems with existing treatments, and they know what they want most from new treatments, not just in terms of longer survival, but quality of life and greater convenience.”
This was music to the ears of the advocates, but did not chime with many of their experiences. HTA bodies don’t really care about quality of life, they look only at survival figures, was one comment. Another said that HTA bodies took little account of their input. “If we ever talk to pharmaceutical companies or accept their funding for our activities, they see our evidence as tainted.” The time taken by HTA reviews was said to be “absurd”, delaying patient access to a new drug they may desperately need. Many felt that HTA bodies put demands on patient groups they are in no position to fulfil. Deb Maskens of the International Kidney Cancer Coalition said that, in Canada, HTA bodies expected them to provide impossible standards of evidence they were not resourced to achieve. “We use the internet and are told it is a biased survey that will not reach, for instance, older patients. We are told to organise focus groups and one-to-one interviews. But if no one is paying for us to do this, is it really valued?” she asked.
“We do value it, and we certainly take account of impact on quality of life,” Paterson responded, though he conceded that attitudes vary from country to country – many European countries give patients no say at all in evaluating new therapies. Patient input, he said, won’t override all the other evidence, but it can certainly sway a decision that is finely balanced. “It could tip the balance in favour of the therapy, or allow sub-groups to be identified – for instance patients whose comorbidities put them at particular risk from side-effects of existing therapies – or it may show extra benefits to the health system – for instance through fewer emergency hospital admissions.”
The Scottish Medicines Consortium does not expect patient groups to produce ‘gold standard evidence’, said Paterson, and it also provides them with some expert assistance. While questionnaires, surveys and focus groups are all valuable sources of information, anecdotal evidence and individual patient stories and opinions also have a role to play.
Suspicion about pharma influence is a problem, he agreed, and it needs gradually to be broken down. “The problem is that there have been examples of bad practice, and then people extrapolate from the bad to the general, and we do need to move beyond that.” The advice given by the Scottish Medicines Consortium is simply to be upfront about any interrelations or sponsorship. As for the time taken to evaluate new therapies, in Scotland they take no more than 16 weeks, he said. “If we can do it, why can’t everyone else?”
In Paterson’s view, the answer to many problems lies in proposals to identify what patients really want from a new drug before it enters phase II or III trials, so that relevant data can be collected and made available to HTA bodies as soon as trials are complete. Patient groups need to be involved at the trial design stage to help identify what data should be collected and how best to go about it. “There will be a need for more patient involvement in both licensing and HTA,” he said. “Patient advocacy groups need to grasp this change.”
“There will be a need for more patient involvement in both licensing and HTA”
Partners in care
As an example of how to go about gathering robust evidence from a large and disparate constituency of patients, Giora Sharf of the CML Advocates Network described a survey they conducted on how well patients stuck to their Glivec prescriptions and the reasons for non-adherence.
This produced a highly influential report, documenting the surprising extent to which patients on long-term medication miss doses, either through forgetfulness or by design, even when their illness is potentially life-threatening. It took a patient group to do this, because patients are often reluctant to admit to their doctors that they have mixed feelings about their medication – especially when the medication in question is a ‘wonder drug’.
Sharf described how they worked with medical and psychology experts to draw up a pilot survey which was translated into eight languages, and distributed online, attracting 150 responses from patients across 10 countries. The results were presented at a major haematology conference, where they won support for a larger scale study. They validated a scale for measuring adherence, translated the survey into four additional languages, set a budget, and employed a logistics organisation company to help with distribution. To control for the bias towards younger and more educated patients associated with administering the survey online, paper versions of the survey were distributed by doctors in three countries and their results compared against online survey results from the same countries.
The final CML advocates network survey received more than 2,150 responses online and almost 400 on paper. It revealed the surprising finding that only one in three patients who responded were “highly” adherent, while more than one in five had “low” adherence – a serious problem given that patients who take less than 90% of the prescribed dose have only a one in five chance of achieving the desired outcome of a “major molecular response”.
The survey flagged the importance of looking beyond serious medical side-effects to learn from patients about what they find most burdensome, whether it be bloating or the endless tyranny of “take 1 with a meal, 4 times a day”. Feedback from independent patient groups is therefore vital not just at the point of evaluating new therapies, but also helping ensure they are used to greatest effect. Feedback from patient groups is vital in ensuring therapies are used to greatest effect
 Partners in research
Partners in research
So long as patients continue to die, establishing an effective relationship with the research community remains a priority. Bettina Ryll, a medical doctor and molecular biologist, talked about how her perspective on clinical research changed dramatically after her husband was diagnosed with advanced melanoma and he participated in several clinical trials. “There is good research and not so good research. When you are dying you need research that gives you the answers you need to make informed decisions on the best treatment options,” she said.
Researchers need to interact directly with patients to better understand their needs, to ensure that efforts and resources are focused on the most clinically relevant issues, said Ryll.
This in turn means patients should be involved right from the inception of a clinical trial, rather than having their role confined to being consulted over the wording of consent forms. Referring to the Helsinki agreement on research ethics, Ryll argued that patients’ interests must take precedence in clinical trials, “And before patients want nice patient information leaflets, they want the chance to survive and see their children grow up,” she said.
Ryll also argued for patient groups to take a more active role in the drugs licensing process – something that is beginning to happen at the level of the European Medicines Agency (see Editorial, page 3). Patients can bring a sense of reality to deliberations over the degree of certainty required about the risk, she says. They have an insight into the benefit of a new drug that represents the only glimmer of hope – however uncertain – to a group of patients with no other options. “We need timely and innovative drugs with a risk–benefit profile that is appropriate for our conditions.” She pointed out that patients with advanced melanoma, where the historic survival rate has been between six and nine months, are likely to accept far higher risk levels than, for instance, people living with CML, who have many well-proven and effective options.
Participants in this Masterclass had clearly been struggling with some of these issues, where they felt they were not technically equipped.
“We’re afraid we don’t have the capacity to be involved on an equal basis with the scientists,” was one comment, to which Ryll responded, “Most scientists value your input. They are highly specialised technical experts who would love to see their work having a positive impact. Go and tell your story – it’s about pointing out the questions, you don’t have to come up with answers.”
“Scientists value your input. They would love to see their work having a positive impact”
Derek Stewart, a survivor of throat cancer who provides expert patient input within the UK National Institute for Health Research, questioned how much knowledge and experience people really need. “All I needed to know was that they weren’t working together and focusing on relevant stuff. Don’t accept slick answers. Simple powerful questions are what is needed.”
Europa Donna, the European Breast Cancer Coalition founded in 1994, has the longest involvement with research of all the groups. They were cofounders of the European Breast Cancer Conference in 2000, alongside EUSOMA (the Society of European Breast Cancer Specialists) and EORTC (the cancer research and trials organisation). Head of Policy Karen Benn related how they had been invited to sit on the scientific committee of the Breast International Group research network, which led to their involvement in MINDACT – “a pro-patient trial” aimed at reducing overtreatment of women with low-risk early breast cancers – where they are now on the steering committee, the legal and ethics committee and the “spreading of excellence” committee.
Europa Donna is currently involved in a broad spectrum of major international collaborative trials and research projects, from treatment of early breast cancer to advanced breast cancer and issues of survivorship. It has also been approached by a number of groups applying to the EU’s Horizon 2020 programme for funding for breast cancer research. “It’s important to evaluate potential research projects carefully,” said Benn, “to ensure that the trial/study answers an important question of interest and of use, and that advocates are involved from the outset and have adequate resources for their involvement.” Getting that seat at the table, she added, is not enough in itself. “Advocates are not there to rubber stamp the materials. You need to ensure the patient’s role is respected, and you need to be attentive and assertive. Advocates need time to study materials in advance, ask questions and participate actively in order to ensure credibility and independence, and provide a real consumer perspective.” Out of its experience, Europa Donna is developing a training module for advocates who serve on trial committees.
Better together
The success stories were inspiring, but Markus Wartenburg, from Sarcoma Patients EuroNet, suggested that cancer patient groups might be more effective if they pooled their efforts. “The international cancer patient community lacks a voice,” he said. “We need coordinated action. We need to talk to the EMA [regulators] and EORTC [Europe’s main cancer trials organisation], to ESOP [the pathologists] and to ESMO [the medical oncologists] and also to the pharmaceutical industry. We need to speak with one voice.”
Jan Geissler, representing the CML Advocates Network, agreed, pointing out that issues such as early involvement in shaping research are relevant to all types of cancer, and it is a mistake to insist that patient experts should stick to just one cancer type. “We can work across diseases,” he said. One suggestion was a forum for patient experts in research that works across cancers. This could not only have the advantage of pooling resources and knowledge, but also make it easier for the patient advocacy community to choose who represents them, rather than leaving it up to regulatory or research bodies to decide who to approach.
All but a handful of participants at the Masterclass were patient advocates, but there were also some representatives from supporting pharmaceutical companies present, and they agreed that fragmentation could be a problem. One industry delegate said, “In Germany alone, there are 20 breast cancer groups, and if we work with one, the others say it is not representative.” They stressed that they find it easier to convince their companies to engage with patient groups on research if they can work with umbrella groups that are widely supported. Sarcoma Patients EuroNet was given as an example of a group with “visible value”. Industry delegates also suggested that patient groups could do more to urge specialists to make the case for companies to involve patients groups more closely.
Some participants, however, felt it was unreasonable to expect groups advocating on more common types of cancer to achieve the level of unity Europe’s sarcoma patient advocates have achieved. They also questioned why patients had to have a single voice, when the industry did not demand the same from clinicians, commenting: “You don’t ask the same of doctors – you ask all of them.”
The skills for the job
Many participants at the Masterclass had played a key role founding the organisations they were representing. None had gone into advocacy for the love of a well-written strategic plan, fund raising, or organisational planning. But patient groups hoping to build strategic partnerships and gain the skills credibility to participate in decision making processes need to attend to these things, and the Masterclass offered an opportunity to address this.
The expertise concentrated in the Europa Uomo delegation – comprised mainly of older men – came in handy here, and they helped organise the sessions on strategic planning and managing risk.
Europa Donna also shared the benefits of their experience. Susan Knox, Executive Director, explained how they sought help from the Boston Consulting Group in 2007 to help them reassess where they were going and how to get there. They needed a strategic review to build on a decade that had seen a rapid rise in the number of member groups across Europe, spiralling activity, and a transformation of the environment in which they were working.
Sustainability is a big issue for many. Advocates from lung and melanoma groups pointed out that in cancers that progress fast and have few effective therapies, a high turnover of patients is inevitable. After a death, family members may be traumatised by the experience and not want to continue their involvement. Patients whose cancers are under long-term control, or apparently cured, may also be reluctant to stay involved, as they want to minimise the impact of cancer on their lives.
This means that patient groups always need to attract new active members. And the question of why patients make contact – or do not –was a key area for discussion. Stigma can be an issue – patients often prefer to make anonymous contact online. Doctors are not good at passing on information about advocacy groups to their own patients – they need to be convinced of the value. There may be an image problem, was another suggestion – people don’t understand what patient advocacy groups do.
The fragmentation of groups in some disease areas can itself be a problem. “In patient circles it seems typical for patients to start new organisations all the time, because they don’t like what is there,” was one view. Others saw this as a strength. “There are different types of organisation that are all close to patients and useful to them. This is to be expected, as patients have so many different problems to deal with, including for instance rehabilitation and return to work. Some problems can be addressed by small organisations that offer support and advice, while others need the strength and efficiency of unified umbrella organisations,” said Francesco de Lorenzo, of the European Cancer Patient Coalition.
There were mixed feelings on whether hospitals should be encouraged to set up their own patient groups; on the one hand it could lead to more patients getting the benefit of support from people who understood what they were going through, but on the other it could lead to further fragmentation and undermine the voice of independent patient groups.
Insiders or outsiders
Everyone agreed on the need to foster a spirit of collaboration. But there was a big question about how to work in a coordinated and streamlined manner without stifling the initiative of individual groups.
This may be one of the big dilemmas for patient groups seeking to maximise their impact. Influencing decisions that shape research agendas, reimbursement and service delivery takes more than ‘input’ and ‘involvement’; it also takes the raw human emotions that only patients and carers can express. Is it possible to work ‘from the inside’ and not be assimilated?
Clifton Leaf, a survivor of Hodgkin lymphoma and an award-winning journalist, concluded the Masterclass by making an impressive case for changing the research culture. “The most powerful change agents, I believe, will be patient advocates who can communicate with clarity and passion what the research process looks like now, what the opportunities for change are – and, perhaps most important, what the human cost is likely to be should we do nothing at all.” The change, said Leaf, must come “from within”. But if patient advocates are to retain the passion and the power to effect that change, they may need to keep one foot on the outside.
“The most powerful change agents will be patient advocates who can communicate with clarity and passion”