Often mistaken for a radiotherapist or medical oncologist, this expert in voice-box sparing strategies has reached out to a wide variety of professionals– most recently actors– in his quest to improve the chances of patients with head and neck cancers.
It’s fitting that one of the world’s most influential specialists on cancers that threaten speech shows a rare understanding of the importance of good communication. Jean-Louis Lefebvre, president of the European Head and Neck Society, worries before our interview that I will not be able to make sense of his ‘French English’. In fact he’s direct, clear and concise. But his concern reflects a knowledge that the way we use words is at the heart of good clinical care.
For patients with head and neck cancers – who often come from marginalised sections of society and are unfamiliar with healthcare systems – it’s completely fundamental says Lefebvre, who has been chief of the Head and Neck Department of the Centre Oscar Lambret at the Northern France Comprehensive Cancer Center in Lille since 1978.
“Because the disease is often advanced, you’re having to talk through with them complex combinations of therapy, talking about PET scans, MRIs, CT scans, biology and endoscopy, often when they’re still in shock after being told they have cancer. ‘Hospital’ is a new and strange word for them. This is a completely different situation than breast cancer, where many women are already well informed through the internet and in magazines. They know they need scans if they have cancer.”
Risk factors for head and neck cancers include heavy tobacco intake, often associated with alcohol abuse. More recently, a link has been uncovered between some types of head and neck cancers and the HPV virus, so oral sex is now believed to be a risk factor too. The result is that the subject is unglamourous and difficult for the media and health information campaigns. It is hardly surprising, then, that two-thirds of head and neck tumours are diagnosed late, and neck tumours are on average 3–4 cm at time of diagnosis.
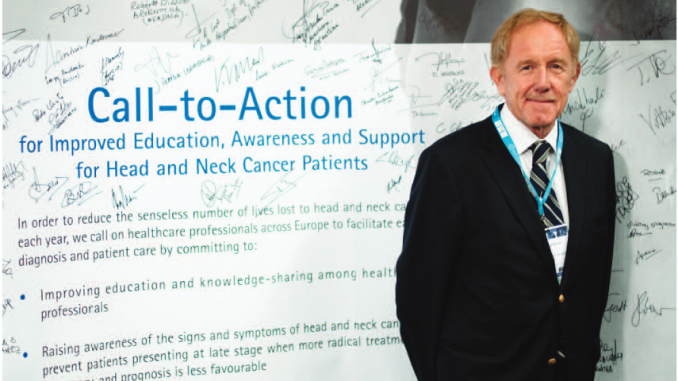
Lefebvre, a surgeon who has become one of the world’s authorities on larynx preservation and multidisciplinary approaches for head and neck cancers, has defined the recent years of his career with initiatives encouraging better understanding of the reasons for late diagnosis and better public awareness for these most unsexy of cancers.
This was manifested most dramatically at last year’s European Multidisciplinary Cancer Congress in Stockholm, where the European Head and Neck Society presented a play, as part of a satellite symposium, about the patient journey. Performed by professional actors, it told the story of Brian – an irascible former businessman, now separated, alone and bitter – who spends his days drinking, smoking and gambling. He is gradually persuaded by his estranged daughter that he should see a doctor about his swollen throat and persistent coughing. There is a telling scene where Brian is told he has cancer and immediately retreats into himself, oblivious to his daughter’s caring enquiries and the doctor’s technical monologue about oropharyngeal tumours, MRIs, ENT and being referred to specialists.
The play, the product of a collaboration between the European Head and Neck Society and pharmaceutical company Merck Serono, was titled Senseless “because of the senseless number of lives being lost through late diagnosis and lack of awareness,” says Lefebvre.
This is not a group of people that are always easy to help, nor do they go out of their way to help themselves. But over his 40-year career, Lefebvre has gone way beyond the role of the surgeon to try to address this. For virtually all that time – apart from brief spells at the start of his career in hospitals in Houston and New York – Lefebvre’s place of employment has been within a square kilometer in Lille, a city in the North of France where the incidence of head and neck cancer is among the highest in Europe. From his office in the Centre Oscar Lambret, he pulls aside a blind to reveal an imposing 1950s block a few hundred yards away that looks like something from George Orwell’s Nineteen Eighty-four. That, he points out, is the University Hospital where he started work as a surgeon.
He was born not far away too, in 1947 in Valenciennes, 40 km south of Lille. Lefebvre’s father died when he was young, and his mother hoped he would become an engineer. But unable to get fired up by maths and physics, he went to medical school instead. At the end of general training at Lille University, his interest in plastic surgery led him to the Ear Nose and Throat Department at the University Hospital. It was there that he rapidly developed an interest in head and neck cancer.
“After studying medicine I knew nothing about head and neck cancer and wanted to know more,” he says. “We’d had less than 20 hours in total on ENT, which is nothing – so I knew head and neck cancers existed, but not much more.”
What happened at the University Hospital between 1970 and 1974 set the tone for the rest of his career. Early on in our conversation, Lefebvre takes out of a cabinet a small framed picture of the man he describes as “my mentor”, and props it in front of me. It is Jean-Jacques Piquet, then head of the ENT department at the University Hospital. With Piquet, Lefebvre worked on a new technique of partial laryngectomy, which gave some patients with larynx cancer the option of retaining part of their larynx (voice box) and avoiding a permanent tracheostomy (opening in the neck for breathing).
Through Piquet he also started to learn about the importance of other disciplines. “Every Wednesday afternoon, a radiation therapist from this hospital, the cancer centre, came over to our department and we would have discussions about the best treatments for head and neck cancer patients,” says Lefebvre, who became senior resident in the ENT head and neck service at the University Hospital. “It was one of the first collaborations between a cancer centre and a general hospital, and I was fascinated by this multidisciplinary approach involving patients. It was very satisfying.”
Unslicing the patient
Joining the Centre Oscar Lambret as a head and neck surgeon in 1976, he discovered the world of the large multidisciplinary team, including surgeons, medical oncologists, radiation therapists, pathologists, biologists and social workers. And when he became deputy director of the centre in 1996 – a post he held for five years – he set about changing the structure of the centre so that the patient became the focal point of this multitude of professionals working together.
At the time, the hospital was organised so that patients worked up the three floors of the hospital – from surgery on the first floor, to medical oncology on the second, to radiation therapy on the third. The management team dismantled the approach, which he says “cut the patient into slices”. They reorganised so that the patient stayed in the same department, with different professionals revolving around them. “They can stay with the people they have got to know, and know where they are. It’s far more comfortable.” It’s an approach that is now interesting other hospitals in France.
“The patient stays in the same department, with different professionals revolving around them”
Already involved in French head and neck study groups, Lefebvre moved into the international cancer scene in the early 1980s. Working as a head and neck specialist at the cancer centre, he was charged with keeping up to date with developments in treatments beyond surgery. He became involved in the main study group on head and neck cancers in Europe at the time, run by the European Organisation for the Research and Treatment of Cancer (EORTC), and was asked to be the chairman in 1989 – a role he continued until 1998.
“I realised there was a need for European collaboration, because I met people with different concepts. Here we were in Latin Europe, where surgery was the main treatment for head and neck cancer. But working with people from Scandinavia, it was clear that radiation and oncology were the main treatments. We had two different philosophies, and we had no idea who was right. So the need for collaborative studies was clear.” This new international collaboration led to him leading far-reaching developments in the treatment of head and neck cancers of which he remains proud.
“We had no idea who was right. So the need for collaborative studies was clear.”
The potential of chemotherapy to treat people with advanced head and neck cancers was just beginning to be understood – Lefebvre remembers hearing the “earth changing” results of two studies reported at ASCO in 1982 showing that a new chemotherapy protocol (cisplatin and 5-fluorouracil) produced impressive response rates in previously untreatable cases of head and neck cancer. “This meant that we now had three partners: the surgeon, the medical oncologist and the radiation oncologist, and now we had to integrate chemotherapy in treatment with curative intent. It was a complete change, and the beginning of another aspect of my career.”
Pioneering personalisation
Lefebvre, among others, used this knowledge to devise new approaches to identify patients for whom non-surgical treatments would work well. “Those patients who were good responders to chemotherapy were also good responders to radiation. So we said: OK, we can use chemotherapy as a way of selecting two groups of patients – those who are still candidates for total laryngectomy, because they do not respond enough to chemotherapy, and those who are good responders, who can move to irradiation.” The result was that total removal of the larynx – and therefore loss of voice and permanent tracheostomy – became no longer necessary for selected patients with advanced cancer.
The work, which he sees as a continuation and logical conclusion of his research into new surgical techniques with Piquet, made him a world authority on larynx surgery, organ preservation and clinical research. He has contributed hundreds of papers, abstracts and chapters, given numerous oral presentations and been invited to lecture throughout the world.
What is ironic, but also indicative of his multidisciplinary outlook, is that he established his authority as a surgeon by promoting non-surgical approaches. “It’s not rare at international meetings that I am introduced as a medical oncologist or a radiation oncologist. Some people don’t think I’m a surgeon, because I discuss all the disciplines and talk about non-surgical treatment!”
He was appointed director of the International Federation of Head and Neck Oncology Societies in 2002 and then president of the International Academy of Oral Oncology. As his profile rose, and with it interest in all aspects of the treatment of head and neck cancers, he realised there was a need for a truly European body to bring together national expertise. Building on networks of head and neck societies already established in northern Europe, he was one of the founders of the European Head and Neck Society (EHNS), a federation of national societies which began holding regular scientific meetings in 2001 and was officially constituted in 2006. Lefebvre is its first president.
Communicating with patients and the public
It was the EHNS that decided to work with Merck Serono (Lefebvre is a member of its advisory board) on finding out more about why so many cases of head and neck cancer were diagnosed late. The result, in 2008, was the ‘About Face’ survey of 7000 people in Europe, which found that public awareness of head and neck cancer was extremely poor. As many as 20% of respondents believed head and neck cancer affected fewer than 1000 people in Europe – one hundredth of the correct figure. Over half (including health workers) incorrectly believed head and neck cancer affects the brain.
For Lefebvre, one of the most important findings was that when people did know something about head and neck cancers, it came not from doctors, but friends, relatives and the media. “This shows that clearly we need to work with the media,” he says.
“When people did know something about head and neck cancers, it came from friends, relatives and the media”
A follow-up survey in 2010 included detailed interviews with patients, and confirmed that communications with doctors were very poor. Merck and the EHNS decided that a symposium including a drama at ESMO would be a powerful way of presenting the issues. The symposium drew 40 journalists from different countries, with Lefebvre providing at least ten press interviews. A follow-up meeting in London attracted similar interest. Now EHNS is considering publishing a brochure in very simple language, and in different languages, aimed at general practitioners, dentists and pharmacists.
Lefebvre realises that the reasons for delays in diagnosis are complex and solutions aren’t easy to find. Research at the Centre Oscar Lambret indicates that 80% of head and neck patients come from the poorest strata of society, 31% live alone at the time of diagnosis, and only a tiny minority are working. These groups have concerns about entering a healthcare system for financial, personal and cultural reasons. Quite often they genuinely believe their symptoms are nothing to worry about, because they have lived with tobacco-induced throat inflammation for a long time anyway.
But he is convinced that more could be done through publicity campaigns. He believes celebrities and public figures are particularly good at bringing previously taboo subjects like cancer out into the open – particularly in Latin cultures, where he says private concerns such as illness are rarely discussed in public. The honesty of film star Michael Douglas talking about his throat cancer has set a positive example, which he’d like to see followed by other celebrities in Europe.
When it comes to supporting these patients once they are in the health system, there’s plenty that health professionals can do. “We have to think about how to organise the process of information-giving from the moment of diagnosis onwards,” he says. At the Centre Oscar Lambret patients are first given very basic information about cancer and their diagnosis, and a simple note for them to read about what happens next. This can be discussed with their physician at the next appointment. There is also a consultation with a nurse a couple of weeks after diagnosis. “It’s much easier for patients with this social profile to openly discuss with a nurse than a physician, particularly if they have ‘Professor’ written on their badge!”
Clinicians also need more guidance on head and neck cancers, he believes – both on clinical research in the field, and communication issues. At Lefebvre’s suggestion, courses on head and neck cancers run by the radiation-oncology society ESTRO will, from this year, include an hour on clinical research, and next year the course will include an hour with a communication specialist, explaining how to communicate bad news to patients. He has also approached the European School of Oncology about the possibility of including communication training in head and neck courses.
Underlying all Lefebvre says is the unshakeable principle that, for all their difficulties, this group of patients is as worthy of respect and professional effort as any other. “They suffer from stigma, but as soon as they become confident in us here, they accept us and what we have to say totally. It is extremely rare for a patient to refuse to sign a consent form to enter a clinical trial. In my whole professional life I have been insulted just twice.”
Now 65, Lefebvre is not facing the prospect of next year’s retirement – and separation from these patients – with particular relish, and expresses mild envy at the opportunities and challenges younger generations will face. “Many things are changing. Now every year we have new approaches – minimally invasive surgery, reconstructive surgery, biotherapies, new radiotherapy techniques. Modern functionional imaging and biology is also bringing new diagnostic tools. Now we have to work to validate all the treatments.
“The goal for the new generation is to work together to find an evidence-based approach to the best options for each patient.”
“I often say, the gold standard of care does not exist. There is only one standard – the multidisciplinary approach, and the role of the tumour board to select from all the variegated options what is best for the individual patient. And if head and neck surgeons want to continue to be chiefs of the orchestra, they must know every instrument.”
“If head and neck surgeons want to continue to be chiefs of the orchestra, they must know every instrument”
Lefebvre has always drawn a strict line between family life and professional life, never mixing the two, protective of his family’s privacy. He has three children, and one daughter is an oncologist – but they never talk shop together, not even when both of them are attending the same cancer conferences. Home is home, work is work. But he isn’t quite sure what he will do when all his time is home time: maybe he’ll take up golf again, travel with his wife, maybe do some more cooking.
He will, he observes, have more time for his grandchildren than he has had for his children. But in a year or so he certainly won’t be lecturing, or doing anything to suggest that he is still one of the world’s leading experts on head and neck cancers. There is an art, he says, to knowing when to leave the stage to others. It will be in good hands.
“You lose your credibility and your contact with the real world when you stop seeing patients on a regular basis,” he says. “In ten years, many things will change, and a new generation will do these things better than I.”