A special multidisciplinary session on ovarian cancer took place during the European Congress on Gynaecological Oncology, in Athens, with the aim of predicting what will happen in the field of ovarian cancer in the near future
During ESGO 21st European Congress on Gynaecological Oncology that took place earlier this month in Athens, Greece, Cristiana Sessa from the Oncology Institute of Southern Switzerland (IOSI) lead an observatory session on ovarian cancer. Its main aim was to get an overview of innovation and care in ovarian cancer through the eyes of the different experts involved — including clinicians, scientists, and patients — and to ask them what they hope or expect over the next 12 months.
“Ovarian cancer is an evolving field,” explained Sessa. “Twelve months is a period of time where things can change very much.”
 Ovarian cancer is the leading cause of death among all gynecological cancers in developed countries, with most patients having advanced-stage tumors. A multidisciplinary team of specialists is the gold standard for treatment, so the session reflected a multifaceted approach, giving the floor to a pathologist, a clinical scientist, a clinical geneticist, a gynecologic oncologist, a medical oncologist and a patient.
Ovarian cancer is the leading cause of death among all gynecological cancers in developed countries, with most patients having advanced-stage tumors. A multidisciplinary team of specialists is the gold standard for treatment, so the session reflected a multifaceted approach, giving the floor to a pathologist, a clinical scientist, a clinical geneticist, a gynecologic oncologist, a medical oncologist and a patient.
Better classification
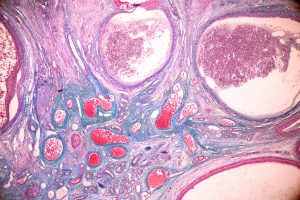
Xavier Matias-Guiu, from the Lleida Biomedical Research Institute (IRBLleida) in Spain, is a pathologist using molecular tools to classify the disease and to offer prognostic tools. He announced that the 2014 WHO Classification of Tumours of the Female Reproductive Organs will be updated in 2020. “We are in the process of writing the next classification, which is going to be published during the next 12 months” he said.
The World Health Organization (WHO) used to update this classification every 10 years, but the pace was changed when they realized that the scientific evidence was accumulating more rapidly than expected, Matias-Guiu explained.
Some upcoming changes will include new common types, such as the mesonephric-like carcinoma, or incorporate rare ‘mixed carcinomas’ after they were identified as an independent group.
There is also some controversy regarding the inclusion of seromucinous carcinomas as a distinct entity, the expert said. In the 2014 WHO Classification, seromucinous tumours were categorized as a new tumor group which were further divided into benign, borderline, and malignant (or carcinomas) — similar to other epithelial ovarian tumors. “Some believe that the seromucinous carcinomas subgroup is just a minor companion of the endometrioid carcinoma, and that’s probably the viewpoint we’ll implement in the next edition” revealed Matias-Guiu.
Checking for both somatic and germline mutations in the tissue
will save time, allow for early treatment,
and save costs in genetic counselling
The expert also tackled the issue of incorporating digital pathology in cancer care centers, which he admitted was a challenge but an essential tool that he expects to spread in the next 12 months. “That means we will leave the microscopes and work on a computer like radiologists” he said. Digital pathology will increase objectivity, and will allow for real-time consultations and accurate quantification of biomarkers, and will also help the creation of diagnostic algorithms using machine learning.
Another challenge will be the availability of an integrated pathology-molecular report, despite some reference hospitals have already implemented it. “In ovarian cancer, we are used to check for germline mutations; now, we are looking for somatic mutations” the expert said. “Geneticists and pathologists should work together to analyze germline and somatic alterations, probably starting with the tissue first.”
Checking for both somatic and germline mutations in the tissue will save time, allow for early treatment, and save costs in genetic counselling, he explained. Only patients who are found to have a tumor mutation will be sent for counselling.
But Matias-Guiu warned that under no circumstances should pathologists “only be tissue providers for someone performing molecular analyses”, and again stressed the need for collaboration.
The genomic of rare disease
Charlie Gourley from the University of Edinburgh, who is investigating the biology of ovarian cancers, provided an insight on the characterization of rare ovarian cancers on a molecular level. Besides the high-grade serous ovarian cancer subtype, the amount of analysis and molecular data available for the other subtypes is fairly small, he said. “What I hope for the upcoming year is a better characterization of the genomic landscape of rare ovarian cancers”.
Gourley detailed the studies and the available molecular data for all rare ovarian cancers: mucinous, endometrioid, clear cell, high-grade serous and low-grade serous. His lab has recently sequenced 112 types of endometrioid ovarian cancers — one of the subtypes that still remains poorly represented — and the data will come out during the next year. “Hopefully there will be other labs that are also doing similar analyses which will allow for cross-comparison” he said.
Over the next year he also foresees improvements in scar assays for establishing PARP inhibitors sensitivity and resistance. “It’s quite clear that the BRCA-mutant patients do extremely well with this therapy, but what about non-BRCA-mutant patients? How can we work out who really benefits?”
Until now, the way doctors select who should be treated with PARP inhibitors doesn’t consider at all the resistance, Gourley notes. Even an HRD+ patient can simultaneously be resistant to PARP inhibitors due to an acquired event such as a second mutation in BRCA1/2 or a BRCA1 methylation. “Our assays will need to be multi-factorial and to include assessments of resistance as well as sensitivity” Gourley stated.
Recommendations for genetic counselling
The most significant risk factor for ovarian cancer is BRCA1 or BRCA2 mutations, responsible for about 10-15% of all ovarian cancers and in BRCA mutated patients the risk is increased also by age. “BRCA 1/2 germline mutations are the strongest risk factors for women to develop ovarian cancer, but at the same time, it’s also true that the majority of the women carrying the mutation will never develop ovarian cancer,” said Emmanouil Saloustros, an assistant professor of Oncology at the Faculty of Medicine of the University of Thessaly, Greece.
Saloustros briefly talked about the surgical risk-reduction recommendations according to current guidelines, and pointed out how various factors apart from genetics — such as age, family history and environment — play a significant role. “I would like to see a combination of all these factors in a model that can incorporate optimal risk stratification,” he said. “Further data on the BRCA1-specific mutation in serous ovarian cancer will help us to better decide on the role of prophylactic hysterectomy, in addition to salpingo-oophorectomy”.
“We need a better access to genetic counselling
for all patients in all countries,
including my own, Greece”
Sometimes genetic tests find a variant of unknown significance (VUS), a gene segment that looks different from the way it is normally expected. This challenges the counselling and the management of the patients, Saloustros said, as it is unknown whether these variants are harmless or actual risk factors. However, the expert believes that more VUS will be re-classified in the next year, determining whether or not women who have these variants will have an increased cancer risk.
The RAD51C gene is another challenging marker, said Saloustros. Although the gene has been linked to the highest risk for ovarian cancer, it is not clear who should be tested for this mutation, who should get surgery to reduce the risk, and what is the risk for the member of a high-risk family who tests negative for the mutation. “More data are needed in order to better decide if this test is really useful and who can benefit from it” he said.
He also said that genetic counselling can be a major issue in other rare forms, reporting the case a family in which both the mother, aged 40, and the older daughter, aged 20, were diagnosed with a rare ovarian cancer (small cell carcinoma of the ovary of hypercalcemic type or SCCOHT), while the youngest daughter was positive for the SMARC-A4 mutation. “We don’t know if we should recommend any risk-reduction surgery to the young girl” he stated. “I hope that in the next year more data on the cumulative risk of ovarian cancer will be available, so we will be able to better counsel the patients and their families.”
And he concluded: “I would like see an increased awareness, among healthcare providers, about the BRCA 1/2-associated ovarian cancer and for the promotion of genetic testing. We should also push for a full reimbursement of this test. We need a better access to genetic counselling for all patients in all countries, including my own, Greece.”
Recommendations for surgery
“We currently have all the tools to perform surgical treatments on patients but we need to guarantee the same level of treatment for all the women with ovarian cancers” said Denis Querleu from the Institut Bergonié Cancer Center in Bordeaux, France, who is also the President of the European Society of Gynecological Oncology (ESGO). He summarized the ESGO recommendations for ovarian cancer surgery in early versus advanced ovarian cancer, highlighting the fact that guidelines are strongly evidence-based and there is no more discussion about the proper protocol to be used.
The actual issue is the quality of care. “In France, 40% of ovarian cancer patients are treated in centers that perform less than 20 surgical procedures of cytroreduction per year” he said. “This means that many patients undergo poor quality surgeries, and chemotherapy is not a backup for a bad surgery”.
Querleu said that there is a need for standardization, and also a need for a better, centralized organization, as it has happened in West Sweden, where patient survival rates have dramatically increased. There is also a need for quality indicators to achieve a basic standard of treatment for all patients. “Not all surgeons and all surgical teams are able to achieve optimal results in patients who could benefit from surgery” he said.
Querleu also mentioned the Hyperthermic Intraperitoneal Chemotherapy (HIPEC), which is performed during surgery in advanced ovarian cancers, stating that we need more studies to figure out whether patients really benefit from it.
New treatments and new definitions
Jonathan Ledermann, a professor of medical oncology at the University College London (UCL), addressed three areas where he thought changes will occur over the next year: the use of PARP inhibitors as first line treatment of ovarian cancer, the re-definition of the terms platinum sensitivity and platinum resistance, and the implications of using PARP inhibitors as a maintenance therapy for recurrent ovarian cancer, especially after they have been used as first line therapy.
Ledermann mentioned three clinical trials (PRIMA, PAOLA-1 and VELIA) that have shown significant progression-free survival benefits of maintenance PARP inhibitors in an intention-to-treat analysis across all patients, irrespectively of BRCA mutations. “The greatest benefits were seen in patients with BRCA mutations, confirming the SOLO-1 data” he stated.
Although these trials answered several questions, they also posed new ones, said Ledermann. The PRIMA study was carried out on patients with poor prognosis without using bevacizumab (the standard of care), whereas the PAOLA-1 study added olaparib to bevacizumab, so the effects of the drugs cannot be disentangled. In the PRIMA study, patients receiving niraparib had a longer PFS than those who received placebo while in the PAOLA study there was no difference in the two groups (bevacizumab plus olaparib versus bevacizumab alone). More questions arise analyzing the effect of niraparib in the PRIMA trial or olaparib in the PAOLA-1 trial on HRd+ and – patients (with or without BRCA mutation), as both show a decrease in efficacy.
Ledermann also discussed the definitions of platinum sensitivity and platinum resistance. “They just don’t make sense, especially as we understand more about the molecular biology of the disease” he said. “How can we say that a tumor is resistant if it relapses within the first 6 months while we say that it is platinum sensitive if it relapses 6 months and one day after the first treatment?” he argued.
Ledermann supported the ESMO-ESGO consensus conference recommendations on ovarian cancer published earlier this year, which suggest avoiding the use of the relapse’s timing to define platinum sensitivity and, instead, to take into account the biology of ovarian cancer. “We need to translate our knowledge into clinical practice, and to move away from rigid definitions that prevent us from using platinum in patients who could benefit from it” he said.
Finally, the expert discussed the development of PARP inhibitor maintenance therapy in recurrent ovarian cancer. In 2014, study 19 was the first to use olaparib as a maintenance strategy in BRCA-mutated ovarian cancer (after platinum-based therapy). A few years later the drug was licensed for the BRCA-mutated population. Shortly after, the same study, together with the NOVA and ARIEL 3 trials, allowed the license to be extended to all patients; in 2019 the license was extended to first line therapy thanks to the SOLO-1 trials results.
“We want to stop ovarian cancer prognosis
being a question of luck”
“This is just the beginning, we are clearly going to see greater changes as soon as the results of the three studies will be submitted to the regulatory authorities” said Ledermann.
A patient’s perspective
 Charo Hierro — a patient advocate and member of ASACO, the Spanish association for women with ovarian and gynecological cancers and their families — took the stage to speak about patients’ expectations and what needs to be changed in the future.
Charo Hierro — a patient advocate and member of ASACO, the Spanish association for women with ovarian and gynecological cancers and their families — took the stage to speak about patients’ expectations and what needs to be changed in the future.
Patients from all over Europe face a number of problems, Hierro said, from diagnosis to treatment. It usually takes a long time to reach a diagnosis due to the non-specific symptoms, and primary care doctors commonly refer the patients to a gastroenterologist. “Diagnosis can take from one month — if you are lucky — to six, seven, or even more months if you are not” she said. “As ovarian cancer is very aggressive, this delay in results in a worsening of the disease.”
80% of patients are diagnosed with stage III or IV ovarian cancers. Because many doctors don’t suspect ovarian cancer when they see patients with symptoms, such as bloating, pelvic or abdominal pain, trouble in eating or feeling full quickly, and urinary urgency, patients groups advise women and GPs to take these symptoms seriously if they persist for more than two weeks.
“Surgery is the only factor that can improve the prognosis” said Hierro. The survival of the patient is strictly connected to the quality of the surgery: it must be carried out by a gynecologic oncologist within a multidisciplinary team; hospitals must have all the necessary equipment and must perform at least 20 ovarian cancer surgeries per year. But gynecologic oncology is not officially recognised as a sub-speciality in all countries and often the team is not specialized, argued the advocate.
Hierro said that doctors have the duty to listen to their patients, and to know how to deal with them in a proper and sensitive manner, encouraging them to ask questions, and providing accurate advice. So all doctors should be trained accordingly, she said.
She also talked about the importance of joining a patient association. “Patients are often reluctant to join an association” she said. “They are afraid and they don’t want to be in touch with other patients. Sometimes they don’t know the benefits they can get, and some are simply not informed about the existence of an association” she said.
To spread their message and as a reminder for doctors, ASACO created the “Stone by stone” initiative: members paint stones with colorful images or uplifting messages, and include the ASACO logo and information. The stones are left in doctors’ offices, public parks or buildings.
Hierro said that associations or advocacy groups representing all gynecological cancers — particularly ovary, endometrial, cervix, vulva and rare cancers — exist in many countries, and most of them are part of the wider ESGO network called ENGAGe (European Network of Gynecological Cancer Advocacy Groups).
The patient advocate ended with a clear expectation for the upcoming year: “We want to stop ovarian cancer prognosis being a question of luck”, she said.





