Precision medicine was meant to see the end of ‘maximum tolerated dose’ as the standard for introducing new drugs. It hasn’t happened, and many patients continue to suffer unnecessary toxicity from overtreatment, with health services picking up the bill. Peter McIntyre asks: who should be responsible for optimising our use of cancer drugs?
Developing innovative anti-cancer therapies is science at its most cutting edge. Learning to use these therapies to best effect is perhaps a bigger challenge – one that many clinicians and researchers believe we are failing.
Physicians, patient advocates and cancer leaders are frustrated at a failure to optimise the benefits of new treatments to extend life while minimising harm.
There is a lack of incentive to design and fund trials to optimise doses, combinations, sequences and duration, and a lack of leadership to make it happen.
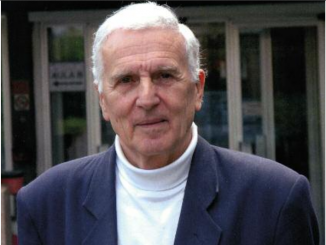
Writing in this issue of Cancer World, Denis Lacombe, director of the European Organisation for Research and Treatment of Cancer, says that current models for developing new therapies are not patient-centred, they are drug-centred, “heavily driven by commercial interests, using a chaotic approach, often without proper analytical validation of assays and inappropriate discriminatory cut-offs for biomarkers.” As a consequence, he argues, “a plethora of expensive agents [are] arriving on the market based on regulatory trials that fail to provide answers to critical questions asked by treating physicians, patients, and those who evaluate and pay for the therapies.”
Lacombe is calling for the system of developing, regulating and evaluating new therapies to be re-engineered in a way that truly places patients at the centre.
He is not the first to raise this issue. At the 2013 Friends-Brookings Conference on Clinical Cancer Research, a group of leading oncologists and regulators in the USA proposed changes to the clinical trials regime, to give greater attention to pharmacokinetics and pharmacodynamics together with better exploration of doses.
Richard Schilsky, ASCO chief medical officer, and Lori Minasian, NCI Deputy Director for Cancer Prevention, co-wrote a briefing paper for the conference with senior members of the US regulatory body, the FDA – ‘Optimizing the dosing of oncology drugs’ – where they argued that the need to develop drugs quickly often takes precedence over the need to find the ‘right’ dose.
At the conference, they made the case that the drug development programme does not adequately evaluate long-term cumulative toxicity, especially for patients who remain on the drug for longer because they are living longer. Lack of information about dosage “often leads to a high rate of dose reductions in cancer clinical trials as well as failure to identify patients who may benefit from a higher dose,” they argued.
Richard Pazdur, Director of the FDA’s Office of Hematology and Oncology Products, told the conference that the cancer research community does an abysmal job of finding the best dose for oncology drugs. “We’ve had this philosophy that ‘more is better’,” but the fact that cancer is a life-threatening disease “does not give us license to… accept such a high degree of toxicity,” (bit.ly/Friends_Brookings_report).
This problem is not new, but the stakes have been raised by significant rates of toxicities associated with new immunotherapy protocols.
The case of advanced melanoma
The most rapid and dramatic advances in cancer treatment have occurred in advanced melanoma, where survival prospects have been transformed by checkpoint inhibitors – first by the CTLA-4 inhibitor ipilimumab and then by the PD-1 inhibitors nivolumab and pembrolizumab. For many patients life expectancy has been extended for years. But the price paid by patients in terms of side-effects can be very high, particularly when they are used in combination, and question marks remain over whether dosage levels are too high and whether longer term maintenance treatment is necessary.
In May 2015 researchers on the phase III double-blind CheckMate 067 trial concluded that nivolumab alone or in combination resulted in significantly longer progression-free survival than ipilimumab alone (NEJM 2015, 373:23–34). Nivolumab was given on permanent (maintenance) doses until disease progression or unacceptable toxicity events, with ipilimumab being given over 12 weeks.
In an update presented at the 2017 American Association for Cancer Research annual meeting (bit.ly/nivo_ipi_update_AACR2017), lead author James Larkin reported that the combination therapy was showing a two-year overall survival rate of 64%, against 59% and 45% respectively for nivolumab and ipilimumab alone.
However serious (grade 3 or 4) treatment-related adverse effects were reported in more than half of patients on the combination arm (58.5%). These included diarrhoea, fatigue, rash, increase in ALT and AST levels, and colitis. Almost one-third of all the patients on the combination arm discontinued treatment (31%), compared with 7.7% and 14.1% in the nivolumab and ipilimumab arms, respectively. However, even in patients who discontinued the combination due to toxicity, Larkin reported that “an impressive survival benefit and responses over 70% were observed.”
Another study, the Keynote-029 phase Ib study, led by Georgina Long from the Melanoma Institute Australia, is looking at a lower dose of ipilimumab in a similar combined therapy, but this time using Merck’s PD-1 inhibitor pembrolizumab in place of nivolumab, with treatment continued for two years or until disease progression or intolerable toxicity.
 In July, Long reported that the trial protocol, which used one-third of the ipilimumab dose used in the CheckMate 067 ipi-nivo trial, showed a “manageable toxicity profile” and “robust anti-tumour activity”, and warrants further exploration. Just over a quarter (27%) had adverse events of grade 3 or 4, which was significantly lower than the 58% in the CheckMate 067 trial, yet a similar proportion (31%) discontinued the combination or one of the component drugs because of adverse events.
In July, Long reported that the trial protocol, which used one-third of the ipilimumab dose used in the CheckMate 067 ipi-nivo trial, showed a “manageable toxicity profile” and “robust anti-tumour activity”, and warrants further exploration. Just over a quarter (27%) had adverse events of grade 3 or 4, which was significantly lower than the 58% in the CheckMate 067 trial, yet a similar proportion (31%) discontinued the combination or one of the component drugs because of adverse events.
Bristol-Myers Squibb is also sponsoring a post marketing trial of other dose combinations of nivolumab and ipilimumab, but that won’t be completed until 2022, while other licence holders are sponsoring combinations of other agents.
Bettina Ryll who founded Melanoma Patient Network Europe and chairs the ESMO Patient Advocates Working Group describes how patient priorities have changed over the past five years. “People were very focused on simply having a chance to get out alive. Now we have drugs that work surprisingly well and people who have no evidence of disease and live for years. Of course everyone is still concerned to survive because we still lose too many, but long term perspectives become very relevant.”
Among the question patients and their doctors need answered, she says, is whether shorter durations could lead to similar survival benefits without the high levels of serious adverse events. “We should never forget that the dosages tested in the original design are not laws of nature. The first dosage is a mouse model and then we do the first in human and then we go to the maximum tolerated dose. Whether that is the right dose or we could be fine with less, we simply don’t know, especially in these new therapies. That is a huge space of uncertainty. There should be a rationale to test this more systematically,” she says.
Decisions on stopping treatment, she argues, need to be based on clinical grounds, which will differ from patient to patient, and she says an increasing number of patients are discussing this with their oncologists. “The patients who are willing to stop are either those whose side effects are so bad they say ‘I would rather die earlier than suffer this’, or people who have had fantastic complete response and the only thing they get are the side effects. People want to step back towards normality.”
Denis Lacombe agrees that the lack of scientific basis for deciding how long immunotherapy treatment should continue is a problem. “The duration of immunotherapy in melanoma patients is a shame because, so far, it is impossible to do this trial and we have absolutely no solid evidence, so doctors interrupt treatment on an empirical basis. I think it is a failure of the whole community, including governments.”
Solo trial “not feasible”
Doctors are keen to see clinical trials carried out to generate solid evidence on the impact of protocols that could make the treatment more tolerable. However, it seems almost impossible for a single centre to go it alone. At the Pisa University Hospital in Italy, consultant oncologist Antonella Romanini launched a small phase II trial to assess response rate, time to progression and toxicity of nivolumab combined with reduced doses of ipilimumab for patients with advanced melanoma. The trial, approved by the Italian medicines agency AIFA and by the area ethical committee, opened for recruitment in March 2017 supported by the Italian Association Against Melanoma.
Romanini says that the aim was to study a lower dose and less aggressive schedule that could also be offered to BRAF-positive patients who had progressed after being treated with BRAF inhibitors. “If you test a combination that is not so toxic you may be able to use it for patients that have very quick progression and are not in very good shape.” The lower dose regime was far cheaper and could, if successful, reduce the costs to the Italian health system.
However, soon after the trial started, the heads of oncology at the hospital told AIFA that they did not think that it was feasible, and the trial stopped.
As company-sponsored trials of combination treatments in Italy are not available in Pisa, Romanini now sends patients to Milan, Genoa or Sienna for treatment, and elderly patients who are too frail to travel have to be treated locally with monotherapy.
She is pressing for the trial to restart, to improve quality of life for patients, but so far without success.
Funding not available
Trials to optimise therapeutic strategies have historically been done by collaborative academic groups, but in the current regulatory and economic environment, and with the high cost of new cancer drugs, that becomes increasingly difficult and the struggle for funding slows progress – and not just for the more rare cancers.
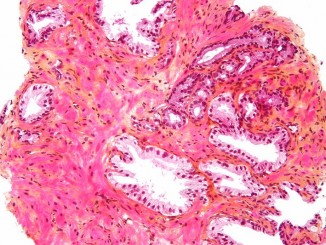
In colorectal cancer, for instance, gastrointestinal cancer specialists have long been concerned at the rate of nerve damage associated with prolonged use of oxaliplatin, which since 2004 has been one of the key components of adjuvant chemotherapy regimens such as FOLXOX and CAPOX (also known as XELOX) that are routinely used in patients with stage III (locally advanced) tumours.
This damage can affect sensory and motor function, with symptoms such as numbness and shooting pains in hands and feet. Clinically meaningful nerve damage (grade 2 or greater) is found in well over 40% of patients using either combination.
In 2007, Alberto Sobrero and a team in Italy proposed a trial to see whether reducing adjuvant treatment for patients with stage III colorectal cancer from six to three months would be as effective with less damage. The proposal led to the establishment of IDEA (International Duration Evaluation of Adjuvant Chemotherapy) – a collaboration that includes six separate trials involving 16 research groups in 11 countries.
By the end of 2013, more than 12,800 patients had been randomised to receive three or six months of either FOLFOX or CAPOX. The final paper is due later this year, but results presented at 2017 ASCO showed that the overall difference in disease free survival on the shorter regimen was less than one percentage point – 75.5% vs 74.6% (JCO 2017; 35S, Late Breaking Abstract 1). For those at low risk of recurrence (defined as cancer spread to 1–3 lymph nodes and not completely through the bowel wall) the difference was even smaller. The rate of serious (grade 3 or 4) nerve damage in patients on the shorter regimen was one-third that reported in patients on the full six months of treatment.
While these results seem intuitively convincing, they did not achieve statistical significance to prove non-inferiority in disease free survival. Despite the statistical near-miss, Thierry André, head of medical oncology at St. Antoine Hospital, Paris, and one of the designers of the IDEA collaboration, says the results have the potential to change clinical practice. “For the clinicians the difference between both arms is very low and the decrease of toxicity is very high and that is very important.”
The trial could potentially improve outcomes for large numbers of patients while making savings on healthcare costs. Yet finding the necessary funding proved a lengthy and time-consuming business. The French study, with 2,000 patients, received €1.6 million from the French National Cancer Institute and the Ministry of Health research programme, PHRC. In Italy funding came from the Italian Health Ministry and in the UK from the UK Medical Research Council. “In each country it was the same,” says André. “It was very tough to find the money and it was really a fight for everybody.”
From planning this trial to reporting results has taken a decade and follow up will continue to assess overall survival.
Some doctors feel industry should do more to support efforts to work out how to optimise the use of their drugs. This has been a point of contention in a Swiss study organised across 37 hospitals and canton cancer centres trialling a shorter duration of treatment with the RANK-ligand antibody denosumab. .
This targeted therapy significantly delays the onset of fractures or events that require surgery or radiotherapy in patients with breast or prostate cancer that has metastasised to the bone. However, it increases the risk of hypocalcaemia, while osteonecrosis of the jaw becomes a serious problem after two to three years of treatment in about 8% of patients, leading to pain, loose teeth and a numb jaw.
The trial aims to recruit 1,380 patients with breast or prostate cancer metastasised to the bone, and will randomise patients to receive either the current maintenance dose of monthly injections or the same dose given every three months.
Roger von Moos, head of medical oncology at Graubünden cantonal hospital and President of the Swiss Group for Clinical Cancer Research (SAKK), says that if the trial is successful, many patients on this long-term therapy will be spared side effects and payers will save millions, given that one dose in Switzerland costs around SF 500 (€ 440).
Recruitment will be completed in 2019, with the outcome known a year later. Progress was slowed because the licence holders Amgen declined to support the trial with finance or to provide denosumab free of charge. Centres in France, Austria, and Greece pulled out because they could not get reimbursement. “We asked Amgen for free drugs for these countries and for some money,” said von Moos. “Afterwards we just asked them for free drugs but we did not get it.”
The trial has only been possible in Switzerland through financial support from the health insurance companies, which will clearly benefit if the trial is positive.
Researchers were disappointed by the response of the pharmaceutical company. “They should be interested to test if there is a schedule that is equally effective but potentially less harmful. If we can diminish the price by alternative dosing, these drugs may become affordable in other countries where they don’t have approval because they are too expensive.”
Who leads and who pays?
The EORTC’s Denis Lacombe is calling for a new approach to organising post-approval dosage trials. “The industry community keeps bringing new, clever and very effective drugs forward but comparative effectiveness research is not really being addressed by anyone. There is no room to improve how we give them in sequence, combination and duration, and to which subset of patients. We have to revisit our framework and systems so that this is properly addressed.”
He suggests two types of clinical trial – regulatory trials to maintain innovation followed by applied comparative effectiveness trials, taking into account how to optimise a new drug into existing therapeutic strategies. “While I would say the regulatory trials are very well known and done by the commercial sector, there is a grey zone around comparative effectiveness applied clinical trials.”
US oncologists and regulators who wrote the briefing note for the 2013 Friends-Brookings Conference proposed something similar – randomised dose comparison studies after the completion of registration trials, prior to marketing approval – a time window when the drug is usually not available to patients – backed with a greater use of patient reported outcomes about tolerable doses.
But while regulators can insist on post-marketing trials, they have limited powers of enforceability – and patients may be reluctant to join trials that vary from accepted dosages. “Post-marketing commitments often cannot be met and are rarely completed within the desired timeframe,” the briefing note authors admit.
In one example, the FDA demanded a post-approval dosage trial after a high rate of dose modifications was noted in the phase III trial of cabozantinib for treatment of metastatic medullary thyroid cancer. The US licence holder Exelixis sponsored a trial of 60 mg of cabozantinib versus the label dose of 140 mg, supported by 30 centres in 10 countries. It opened in 2013 but by September 2017 had not yet recruited its target of 188 patients. If the completion date of March 2018 is met, results will arrive more than five years after the higher dose was approved.
Reducing the risk of neuropathy
Neuropathic damage from oxaliplatin can cause shooting pains, numbness, or even impaired motor function, particularly in hands and feet, which can make everyday tasks difficult. The IDEA trial found that, in patients with stage III colorectal cancer, halving the duration of adjuvant treatment with oxaliplatin-containing regimens, from six to three months, cut the rate of serious (grade 3 or 4) nerve damage by two thirds, with a very minor impact on disease free survival.
In Europe, an opportunity for better addressing some of the optimum use questions may be opening up with the involvement of the European network of health technology assessment bodies (EUnetHTA) in discussing the set up of regulatory trials, as HTA bodies often feed into national processes for assessing the value of new drugs and decisions on reimbursement.
Since July 2017, the EMA and EUnetHTA have been conducting early (pre-registration) consultations with pharmaceutical companies in parallel “to help generate optimal and robust evidence that satisfies the needs of both regulators and HTA bodies”. Companies can discuss with regulators and HTA bodies the setup of phase III trials and, in particular, what they will use as a comparator, the endpoints for the trial and which sub groups of the patient population will be included.
The EMA and HTA bodies have been seeking fuller disclosure from companies on evidence generated during drug development in the lab as well as in early trials, saying that this will also give companies a better understanding of what is needed to achieve marketing authorisation and reimbursement.
The director of EUnetHTA, Wim Goettsch, from the National Health Care Institute (ZIN) in the Netherlands believes there has to be a stronger European HTA voice. “It is becoming more and more important that we have much earlier discussion with the manufacturer on which clinical trial we need in terms of data before making reimbursement decisions on a national level.”
“If you do this at the national level the influence you have on the trial setting will be limited. If we have one European voice to say what we need from the HTA perspective, this influence can be much bigger. That is a crucial starting point, and I think we are going to invest a lot of activity in the coming two years in that perspective.”
The EUnetHTA approach is led by the French Haute Autorité de Santé (HAS) France, and the Federal Joint Committee (G-BA) from Germany. EUnetHTA also has an early dialogue working party with representatives from Italy, the UK, Netherlands, Belgium, and Hungary, soon to be joined by Spain.
EUnetHTA members are piloting three assessments of new cancer drugs and Goettsch says they are insisting on full disclosure. “We have been very specific that they have to provide all the information which they have available and we should be allowed to use those for the assessments.”
There are many reasons why data can be blocked. As part of the Get Real project EUnetHTA attempted to obtain data from registries in three European countries on one cancer as a test run to see if these could be used in joint studies across Europe, but were unable to get the information because of procedures in place to protect confidentiality. “There are a lot of process bureaucratic reasons why it is very difficult to obtain data. We are moving, but very slowly.”
As well as seeking to speed up joint assessments, EUnetHTA intends to continue to evaluate benefits and risks after a product is on the market. This could lead HTA bodies to ask for additional data from pragmatic trials in a real life setting.
“The challenge then,” says Goettsch, “is how are you going to pay for these clinical trials? Who is responsible for that? Sometimes you can still say it is the responsibility of the company. They want to get reimbursement for these drugs and therefore they should also link to what is happening in these countries. This is something we are currently discussing. There is no real answer for that, but I think it is a real issue.”
One avenue is to seek support from research funds and other public sources within countries, as the IDEA trial finally managed to do. “If we can show that it will actually lead to savings for the healthcare system there might also be willingness from the healthcare system to invest some money in this.”
He hopes that the EU will grasp the nettle after 2020 and support European collaboration on health technology assessments with structural rather than project funding.
Von Moos, of the Swiss Group for Clinical Cancer Research, says that national payers – whether governments or insurance systems – need to be more active in supporting trials that could result in lower dose therapies and huge savings.
“For me it is quite clear. This should be in the interests of payers. In the best cases they can increase the standard of care and they can save money and make modern drugs available for populations who just cannot afford these kinds of treatments.”
Supporting these trials will send a signal to the companies that payers are prepared to challenge label dosage if they think the alternatives have not been properly tested. “The payers have an interest and the power to prove whether the pivotal trial or the design of a trial was really ideal. EMA and HTA should have an influence on the study design before the trial is starting.
“We have to invest much more money in early clinical trials, not only to find the maximum tolerated dose but the optimal dose.”
Bettina Ryll, from Melanoma Patients Network Europe, argues it is unrealistic to expect industry to take responsibility for post marketing refinements. “Why should a manufacturer spend money on a clinical study to sell less product in the end?” She also doubts the value of randomising dosage trials when what is needed is smarter data capture and analysis in long-term follow up.
She applauds initiatives such as the Dutch Melanoma Treatment Registry, a nationwide registry that collects data from all melanoma patients to provide insights regarding subsets of patients who benefit from the new drugs.
Ultimately however, the buck stops with national healthcare systems. “In the end it is the state healthcare system that pays for the drugs used in the country, so having access to data showing whether what you are doing works or not makes totally good sense to me. I would not allow national healthcare systems to chicken out of their responsibilities. In the end it is our money – it is tax money or contributions to health insurance that is spent on therapies.”
Optimisation trials: why payers should get involved
S ide effects can reduce the value for money of a therapy in two ways: patients derive less benefit due to reduced quality of life, and there are additional costs associated with any additional care.
In the case of the nivolumab-ipilimumab combination, such is the impact of the side effects that one health economics study estimates that the additional cost per quality-adjusted year of life (QALY) gained with the combination treatment is more than twice the additional cost per QALY gained from using the same treatments sequentially (JCO 2017, 35: 1194–202).
The study modelled a hypothetical cohort of patients, mirroring the characteristics of patients in five phase III trials using more than one of ipilimumab, pembrolizumab and nivolumab for BRAF wild-type advanced melanoma.
The researchers obtained data on rates for drug discontinuation, frequency of adverse events, disease progression, and death. Treatment costs related to side effects (drug costs, physician time, and hospital admissions), which were estimated from US Medicare and Medicaid reimbursement rates.
Compared with the first-line dacarbazine treatment strategy, nivolumab followed by ipilimumab produced an incremental cost effectiveness ratio (cost per QALY gained) of $90,871/QALY, while first-line nivolumab + ipilimumab used in first line, followed by carboplatin plus paclitaxel chemotherapy, produced an incremental cost effectiveness ratio of $198,867/QALY.
Using nivolumab or pembrolizumab as a first line treatment was the most cost-effective option. Combining nivolumab+ipilimumab was the least cost-effective strategy. Reserving ipilimumab as a sequential second-line option rather than in combination was associated with improved patient quality of life, fewer serious adverse effects and a lower rate of drop out. The study suggests that lower dosages can produce most of the benefits at lower cost.
The importance of evidence on the risks and benefits of using drugs in different doses, combinations and sequences for getting the best value for money from stretch health budgets is an argument for payers – governments and insurers – to take some responsibility for optimisation trials.