Brain metastases are an unmet need in current oncologic care. New hopes come from the characterization of their genomic evolution and from the study of circulating tumour cells
Hearing the doctor say that the tests have discovered metastases, for a cancer patient, sounds as hearing a death sentence. Alongside the fear of dying, patients are terrified of the effects produced by the evil lump growing in their brain: “Will I lose my mind? Will I lose control of my body functions?”. Brain metastases (BMs) occur in 20-40% of patients with cancer. Actually, BMs are the most frequent intracranial tumours: the incidence of newly diagnosed BMs is 3-10 times the incidence of newly diagnosed primary malignant brain tumours. Notably, the incidence of BMs is increasing, possibly as the result of the combination of improvements in diagnostic tools and increased survival of patients with solid tumours. The three tumours more likely to metastasize to the brain are lung cancer (36-64%), breast cancer (15-25%), and melanoma (5-20%). More than 6 out of 10 patients with BMs become symptomatic. Neurologic symptoms include headache, focal neurological deficits, and seizures. Patients with multiple metastases and/or increased intracranial pressure can present impaired cognition and altered mental status and clinicians should always suspect BMs in any cancer patient who presents with new neurologic symptoms.
Neglected patients?
The diagnosis of BMs drastically worsens long-term survival rates and the presence of multiple metastases represents a poor prognostic factor. Thus, it is not surprising that patients with BMs have been excluded from most clinical trials. This exclusion, together with the lack of preclinical models that recapitulate the clinical setting, has hampered progress.
Undeniably, randomised trials in patients with BMs are difficult to perform: patients are in an advanced stage of disease and very often are heavily pre-treated. “However, due to the improvement in systemic therapies and better systemic control, a number of patients remain in good clinical condition for an extended period of time. Therefore, prospective clinical trials in a selected patient population could be feasible” says Ahmad Awada, from the Université Libre de Bruxelles (Ther Adv Med Oncol 2018, 10:1–10). The American Society of Clinical Oncology (ASCO) BMs working group has proposed to include in clinical trials “patients with treated and stable BMs for at least 4 weeks or patients with active BMs in early phase trials when there is a strong scientific rationale for probability of benefit”.
The RANO-BM (Response Assessment in Neuro-Oncology Brain Metastases) group, an independent, international, collaborative effort to improve the design of clinical trials in patients with brain metastases, has recently published new guidelines in Lancet Oncology (Lancet Oncology 2018, 19(1):e20-e32).
These guidelines make detailed recommendations on when patients with BMs from solid tumours should be included or excluded in clinical trials of systemic agents. “Neurological, neurocognitive, and quality of life (QoL) reporting should be part of the trial design” highlights Awada. “Considering the current failure rates of existing treatments and the impaired QoL, an interesting approach would be to focus on primary prevention, and secondary prevention, avoiding or delaying the next CNS event and associated symptoms after a first CNS metastatic event”.
The same, but different
The likelihood of CNS activity of the investigational drug is one of the main aspects that should be considered in the decision to enrol BM-bearing patients in a clinical trial. For many years, tumours growing in the brain, including metastases, were considered completely inaccessible to systemic drugs because of the existence of the blood-brain barrier (BBB). In fact, the three pillars of BM treatment are surgery, radiation therapy, and, more recently, radiosurgery. However, over the past decade, researchers have demonstrated that the BBB is disrupted in macroscopic BMs, resulting in increased exposure to systemic agents. Moreover, radiotherapy can induce an increase in BBB permeability, although unpredictable.
The identification of drugs able to cross the BBB paves the way for multimodality treatment approaches, combining surgical resection, radiotherapy, and targeted therapy. The premise for targeted therapy is the genomic characterization of BMs. But what do we know about BM genomics? Recent work contributed to explaining why, besides the difficulty in reaching the tumour, systemic therapies have inadequate control of BMs.
In a comprehensive genomic study (Cancer Discov 2015, 5(1):1-13) of 104 matched brain metastases and primary tumours, published on Cancer Discovery, investigators mapped out the phylogenetic relationship between brain metastases and primary tumours. Priscilla K. Brastianos, from the Harvard Medical School, demonstrated that the primary tumour and BM shared a common ancestor, but had a significant divergent evolution. “We found that 53% of patients harboured a potentially clinically actionable alteration in the brain metastasis that was not detected in the clinically sampled primary tumour” says Brastianos. “Because more than 50% of patients with brain metastases will die of intracranial progression, targetable alterations present in cancer subclones specific to the brain metastasis represent an important opportunity for novel targeted therapeutic strategies to affect overall survival”. The study provided additional relevant information on genetic heterogeneity of BMs. “Although genetically divergent from samples of their primary tumour, intracranial metastases were remarkably homogeneous with respect to driver and/or potentially targetable alterations” explains Brastianos. “Practically, this homogeneity implies that, when clinically available, characterization of even a single brain metastasis lesion may be more informative than that of a single primary tumour biopsy for selection of a targeted therapeutic agent”.
Of note, regional lymph node and distal extracranial metastases were not a genetic surrogate for clinically actionable alterations in the BMs. Several targeted therapies have been evaluated in subsets of patients and demonstrated a significant impact on disease control, survival, and quality of life (QoL). The main molecular targets exploited so far are EGFR and ALK in lung cancer, HER-2 in breast cancer, and BRAF in melanoma. Overall, the response rates to targeted agents in specific molecular subtypes of BMs seem higher than those observed after conventional chemotherapy.
New pathways that are currently under investigation are PI3K and CDK. It surprises no one that there is a lot of excitement about the possibility to use immune checkpoint inhibitors to treat BMs. Ipilimumab (anti-CTLA-4) and pembrolizumab (anti-PD-1) have obtained favourable intracranial response rates in phase II studies conducted in melanoma and NSCLC patients.
Go and find those cells!
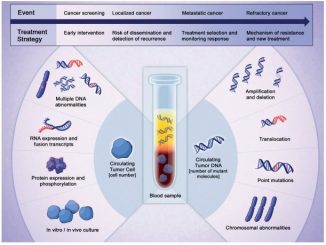
As discussed, the genomic characterization of the primary tumour alone may miss potentially clinically significant alterations in BMs. The analysis of circulating tumour cells (CTCs) or cell-free DNA, from either blood or cerebrospinal fluid, the so-called “liquid biopsy”, would be of an exceptional value to overcome this issue.
Dario Marchetti, director of the Biomarker Research Program at the Houston Methodist Research Institute, has a longstanding interest in the study of CTCs. In 2017, his group reported that CTCs associated with breast cancer brain metastasis are enriched in a distinct sub-population of cells identifiable by their biomarker expression and mutational content. The results of the study, published in Nature Communications (Nat Comm 2017, 8:196), demonstrated the existence of a “circulating tumour cell gene signature” that is distinct from primary breast cancer tissues. From a practical point of view, CTC biomarkers may become a formidable screening tool. “I am a firm believer of the power of CTC biomarkers and CTC-based liquid biopsies to be used one day for the prediction/prevention of cancer metastasis in general, brain metastasis in particular” says Marchetti. “CTC detection/liquid biopsies will not substitute for MRI; rather, they will complement it as a more sensitive detection of nascent metastasis (that is micrometastatic disease), something that MRI currently cannot detect” he replies to the question on whether this approach will substitute neuroimaging techniques. Then he adds: “This approach would be feasible in low resource settings as a diagnostic tool potentially substituting MRI, if MRI costs cannot be afforded. Using relatively low-cost equipment, like a RT-PCR thermocycler and few related supplies, a CTC gene expression test could provide a first approximation value for the presence of metastatic cancer and the high-risk predicting cancer metastasis in the patient”.
While other groups are working on the characterization of lung cancer’s CTC biomarkers, Dario Marchetti’s group is now focusing on melanoma’s CTC isolation. He has recently published an article in Cancer Research (Cancer Research 2018, 78(18):5349-5362) providing first-time evidence that the asymptomatic phase of metastatic melanoma can be recapitulated in vivo using patient-isolated CTCs. If all goes well, in the very near future validated panels of biomarkers will be available to be used as routine tests for the early detection of BMs. And the isolation of CTCs associated with BMs will allow the identification of metastases’ oncogenic driver mutations for the selection of the appropriate therapeutic agent and provide valuable information regarding treatment response and progression.





Leave a Reply