The patient rejects the standard of care. The oncologist cannot answer his question How long do I have? Is the treatment course they agree on second best, or best?
This article was first published online in The Oncologist on 8 May 2015, and is reproduced with permission. 2015 ©AlphaMed Press doi:10.1634/theoncologist.2015-0047
We met almost three years ago. I was in the first year of haematology and oncology fellowship training. He was in his early 60s and had recently retired. His primary care physician had referred him for evaluation of incidentally detected monoclonal proteins. Over the next few days, the workup unfolded. His skeletal radiographs showed lytic lesions, and his bone marrow biopsy showed sheets of plasma cells inundating the marrow space. It was multiple myeloma, a malignancy of plasma cells. I explained to him how these cells, which manufacture antibodies under normal circumstances, had mutated into bone-eating parasites and that his bones had become susceptible to fracture and collapse, like a fort attacked from within.
 A prognostic panel showed that he had one of the most aggressive types of multiple myeloma, defined by deletion of chromosome 17p. Patients with this subtype often need aggressive treatment, respond poorly to treatment, and have worse outcomes. Once the diagnosis sank in, he asked me, “How long do I have?”
A prognostic panel showed that he had one of the most aggressive types of multiple myeloma, defined by deletion of chromosome 17p. Patients with this subtype often need aggressive treatment, respond poorly to treatment, and have worse outcomes. Once the diagnosis sank in, he asked me, “How long do I have?”
Given his disease burden, it was clear (to me) that he needed to be treated. The unfavourable genetic profile of his disease conveyed a sense of impending crisis. However, there was a catch. He had few symptoms, if any, and was in a wonderful overall state of health. His only complaint was mild lower back pain. Most important, he did not want any treatment that would affect his quality of life.
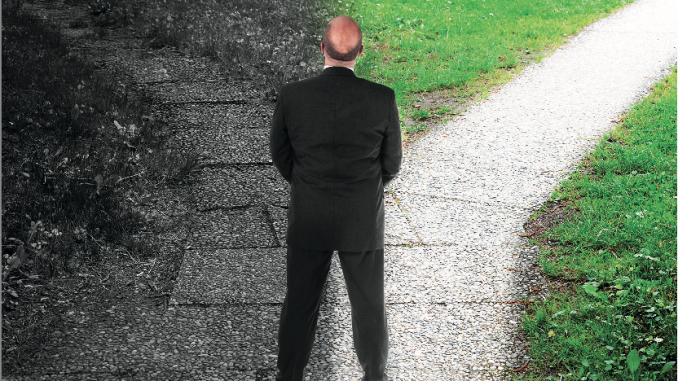
Whereas I sought to protect his excellent health through treatment, he did not think he needed to be treated. We had hit a philosophical roadblock. Optimal treatment consisted of multidrug therapy followed by autologous stem cell transplant. As we discussed treatment-related side effects, his anxiety became palpable. It was clear that although we viewed this treatment as a “standard” approach, he viewed it – especially the transplant part – as extremely toxic.
He was truly concerned about being hospitalised or missing out on a cruise with his wife or skipping a weekend with his grandchildren. What mattered to him were “not the years in his life, but the life in his years.” I sensed his reluctance to proceed, but without treatment, he was at significant risk for disease-related complications like kidney damage, spontaneous fracture of his bones, or paralysis. I felt that some treatment was probably better than none.
We negotiated, and he agreed to be treated, but only with two drugs, and refused the transplant. As expected, this milder treatment programme did little to reduce his monoclonal protein level. Unexpectedly, for him at least, it caused no significant side effects, and given how well he tolerated it, he agreed to try our originally recommended regimen, which consisted of three agents.
Once on the triple-drug regimen, his disease burden plummeted and then plateaued at a low level, which I viewed as particularly concerning, especially in light of the aggressive nature of his disease. It was at this point that we reintroduced the recommendation for a stem cell transplant; however, as before, each conversation about transplantation seemed to further strengthen his resolve not to have it. After another round of negotiation, we were able to collect his stem cells and freeze them for possible future transplant. He opted to continue the triple-drug regimen and tolerated it without any appreciable side effects.
Each conversation about transplantation seemed to further strengthen his resolve not to have it
Once we got over the ‘hump’ of transplant, he seemed more at peace at subsequent visits, probably because he had avoided it. I was also more at peace because, even though he refused a transplant, at least we had access to his stem cells, deep frozen. I continued to see him in the clinic until I finished my fellowship in the summer of 2014. We have kept in touch since then, and he continues to do well.
It has been almost three years since he was first diagnosed, and although his myeloma has not been eradicated, his disease burden and the extent of bone damage have remained stable. Although I am still unsure whether his decision to forgo transplantation was the ‘right’ one, it made me appreciate the questions that come up quite often in the life of an oncologist: How do you define the ‘best’ treatment? What should drive cancer care: the years in a patient’s life or the life in those years? Did I treat him, or did he teach me?
How do you define the ‘best’ treatment? Did I treat him, or did he teach me?
In the story of my patient, I see the amazing story of multiple myeloma. Once a death sentence, myeloma patients are living much longer now. Over the past few years, myeloma research has reached an unprecedented level of advancement. The number of approved therapies for treatment of myeloma is expanding, and drugs like bortezomib and lenalidomide have transformed the landscape of survival. In addition, two more promising drugs, pomalidomide and carfilzomib, were recently approved for refractory myeloma.
Despite our progress, stem cell transplantation is still one of the best available tools for treating multiple myeloma; however, with the advent of targeted and less toxic therapies, it is likely that we will continuously re-evaluate its role in myeloma. Even after his disease stabilised, my patient often asked me, “How long do I have?” Every time, I would tell him I honestly did not know. I loved that answer.
Acknowledgements: Thanks to Robert Aronowitz and Ambika Chikarmane
Affiliation: Dhillon Wishwdeep is affiliated to the Arizona Center for Cancer Care, Gilbert, Arizona