
After the European Medicines Agency (EMA) approves a new cancer drug, reimbursement decisions by each country’s health authorities can take up to one year, with wide variations between countries. according to a study just presented at ESMO 2018 Congress in Munich (Germany).
Kerstin Vokinger from University Hospital of Zurich, Switzerland, and Harvard Medical School, Boston, USA, and her colleagues analysed the fate of all 47 new cancer drugs approved for solid tumours through the centralised European procedure between January 2007 and December 2016, and measured the time between EMA approval and reimbursement decisions, based on health technology assesment studies in four European countries: England, France, Germany and Scotland.
Health technology assesment is defined as “the systematic evaluation of properties, effects, and/or impacts of health technology. It is a multidisciplinary process to evaluate the social, economic, organizational and ethical issues of a health intervention or health technology. The main purpose of conducting an assessment is to inform a policy decision making”.
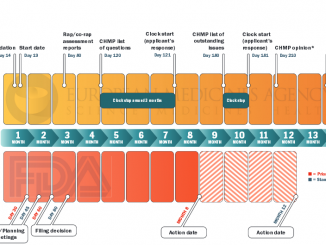
According to the analysis presented at ESMO (that will soon appear in a supplement of the Annals of Oncology), the median time from EMA approval to HTA decisions was two to three times longer in England (405 days) and Scotland (384 days) compared to Germany (209 days) and France (118 days).
“In contrast to the centralised approval of anticancer drugs by the EMA, the time to HTA decisions remains a national responsibility” explainaìs Vokinger. “Among other things, the different amount of resources invested in such assessments and different national regulations regarding HTA systems may lead to variation in the time from EMA approval to HTA decisions in different countries.”
The study found that health authorities generally made decisions much more quickly for drugs ranked as being of “highest benefit” on the ESMO Magnitude of Clinical Benefit Scale (ESMO-MCBS) compared to those with less clinical benefit. However, the variation in time from EMA approval to HTA decisions remained between different countries for these “highest benefit” drugs.
The ESMO Magnitude of Clinical Benefit Scale (see also Too high or too low? ESMO’s clinical benefit scale fuels debate over approval thresholds) uses a rational, structured and consistent approach to grade the magnitude of clinical benefit that can be expected from anti-cancer treatments. “Lowest benefit” refers, for example, to drugs increasing median progression-free survival by a few weeks, whereas the category of “highest benefit” is given to drugs improving long-term survival in the neo/adjuvant setting.
“It is reassuring that in the countries studied, anticancer drugs with greatest clinical benefit on ESMO-MCBS (version 1.1) are associated with faster times to HTA decisions and nearly all are approved for reimbursement” commented Elisabeth de Vries, Medical Oncologist at the University Medical Center Groningen, Groningen, The Netherlands, Chair of the ESMO-MCBS Working Group. “Hopefully, this information can be helpful to raise the interest of HTA agencies in their performance and timeframes.”




Leave a Reply