Selected reports edited by Janet Fricker
Leisure time physical activity is inversely associated with CRC mortality
=> Journal of Clinical Oncology
For patients with colorectal cancer (CRC) leisure time physical activity (LTPA) both before and after diagnosis is inversely associated with all-cause mortality, an analysis of the National Institutes of Health (NIH) American Association of Retired Persons (AARP) Diet and Health study has found. The amount of TV watched both before and after diagnosis, the investigators showed, was associated with mortality.
Physical inactivity has been associated with higher mortality among survivors of CRC, but the independent effects of pre- versus post-diagnosis activity remain unclear. It is known that 55% of CRC survivors report watching more than three hours of TV per day, but whether TV viewing is associated with mortality among survivors of CRC has not been defined.
In the current study, Hannah Arem, from the National Cancer Institute, in Bethesda, Maryland, and colleagues analysed the associations of pre-diagnosis and post-diagnosis LTPA and TV viewing with overall and disease-specific mortality among patients with CRC. For the analysis the investigators used data from the NIH AARP Diet and Health study, which between 1995 and 1996 persuaded 566,398 AARP members, aged 50–71 years, residing in one of six US states or two metropolitan areas, to complete a baseline questionnaire including sections on diet and lifestyle. Follow-up questionnaires on topics such as risk factors were mailed out periodically. Links were made between cohort members and state cancer registries. Participants reported LTPA hours per week using categories of never, rarely, <1, 1–3, 4–7, and >7 hours per week. TV viewing was assigned categories of 0, 0–2, 2–4, and >4 hours per day.
Of the 300,352 men and women considered at risk for CRC, 4,685 CRC patients were identified and 1,541 deaths occurred When survivors of CRC reporting >7 h/wk of pre-diagnosis LTPA were compared with those reporting no LTPA, investigators found a 20% lower risk of all-cause mortality (HR=0.80; 95%CI 0.68– 0.95; Pfor trend =0.021). When survivors of CRC reporting >7 h/wk of post-diagnosis LTPA were compared to those reporting none, they had a 31% lower risk of all-cause mortality (HR=0.69; 95%CI 0.49–0.98; Pfor trend =0.006), independent of pre-diagnosis activity. In comparison with subjects who watched 0–2 h/day TV before diagnosis, those reporting >5 h/day after diagnosis had a 22% increased all-cause mortality risk (HR=1.22; 95%CI 1.06–1.41;Ptrend =0.002), and more post-diagnosis TV watching was associated with a non-significant 25% increase in allcause mortality risk (HR 1.25; 95%CI 0.93– 1.67; Pfor trend = 0.126).
“Because surveys of survivors of CRC have shown a high prevalence of physical inactivity and TV viewing, these findings present an opportunity for clinicians to encourage behavioral changes to positively impact longevity,” write the authors.
Putative biological mechanisms to explain associations between sedentary time, physical activity, and mortality, they add, include physical activity increasing insulin sensitivity and higher circulating insulin and insulin-like growth factors being associated with angiogenesis, tumour growth and anti- apoptotic activity.
- H Arem, R Pfeiffer, E Engels et al. Pre- and post diagnosis physical activity, television viewing, and mortality among patients with colorectal cancer in the National Institutes of Health–AARP Diet and Health Study.JCO2014 doi:10.1200/ JCO.2014.58.1355
Physicians reluctant to follow studies recommending withholding treatment
=> Cancer
Despite the publication of a randomised phase III trial supporting omission of adjuvant radiotherapy in elderly women with early-stage breast cancer treated with lumpectomy and adjuvant therapy, nearly two-thirds of this group of patients continue to receive radiotherapy.
In 2004 the Cancer and Leukemia Group B (CALGB) 9343 trial established lumpectomy and adjuvant therapy with tamoxifen alone rather than both radiotherapy and tamoxifen was a ‘reasonable’ treatment for women older than 70 years with stage 1 oestrogen receptor-positive breast cancer. The study showed a five-year local recurrence rate of 1% in the group receiving adjuvant tamoxifen plus radiotherapy compared to 4% in the group receiving tamoxifen only following breast conserving surgery. Omission of radiotherapy, however, has not been widely adopted into clinical practice. A publication evaluating a Medicare database of 13,000 women showed minimal changes in clinical practice following publication of the CALGB 9343 trial.
In the current study, Manisha Palta and colleagues, from Duke University in North Carolina, set out to look beyond Medicare to a SEER database based on geographic regions representing 28% of the US population. “SEER data are likely representative of national practices and not biased by the philosophies of particular academic institutions,” write the authors. For the study involving 40,583 women older than 70 years with T1N0 hormone receptorpositive breast cancers, receipt of adjuvant radiotherapy after breast-conserving surgery was compared between those receiving treatment in the period 2000 through 2004 (before publication of the CALGB 9343 trial) and those receiving treatment in the period 2005 through 2009 (after publication).
Results showed that 68.6% of patients (n=12,881) treated in the earlier time period received some form of adjuvant radiotherapy compared with 61.7% (n=13,440) treated later (P<0.001). Additionally implant radiotherapy was used for 1.4% of the population in the earlier time period compared with 6.2% treated later (P<0.001). Results analysed by age group demonstrated that radiotherapy was administered less frequently to older women, with approximately 30% of patients aged over 85 years receiving adjuvant radiotherapy compared with more than 75% of those aged 70–74 years.
An earlier assessment of the impact of tamoxifen administration within the National Comprehensive Cancer Network institutions, by contrast, demonstrated that after publication of randomised trials, use of tamoxifen increased from 24% to 45%. “Evidence suggests that the medical community may react differently to withholding treatment compared with adding a new treatment,” write the authors.
One possibility, they suggest, is that financial incentives, either on behalf of the health system or practitioners, may contribute to the difference, with physicians incentivised to favour treatment over no treatment, particularly when either option is considered appropriate.
Use of patient decision aids for older women considering adjuvant radiotherapy after lumpectomy, add the authors, would be beneficial to enhance patient knowledge and allow them to be better informed about treatment options.
- M Palta, P Palta, N Bhavsar et al. The use of adjuvant radiotherapy in elderly patients with early-stage breast cancer: changes in practice patterns after publication of Cancer and Leukemia Group B 9343. CancerJanuary 2015, 15:121:188–193
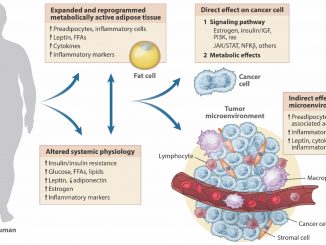
Nearly half a million cancers a year worldwide attributed to obesity
=> Lancet Oncology
Worldwide nearly half a million new cases of adult cancer in 2012 could be attributable to high body mass index (BMI), found a population-based study by the WHO’s International Agency for Research on Cancer (IARC). The proportion of cases was greater among women than men and in highly developed versus less developed countries.
Recent statistics have shown that 35% of adults worldwide aged 20 years and older are overweight (BMI ≥25 kg/m²), including 12% classified as obese (BMI ≥30 kg/m²). Studies have also confirmed associations between high BMI and risk of oesophageal adenocarcinoma and colon, rectal, kidney, pancreas, gallbladder (women only), postmenopausal breast, ovarian, and endometrial cancers.
In the current study Melina Arnold, from IARC, and colleagues, set out to estimate the global burden of cancer incidence in 2012 attributable to high BMI in 2002, acknowledging the 10-year time lag between exposure to high BMI and outcomes. BMI estimates from 2002 were taken from the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group, while the GLOBOCAN 2012 database of cancer incidence and mortality for 184 countries was used to estimate the numbers of new cancer cases attributable to high BMI.
The investigators estimated that, in 2012, 481,000 (3.6%) of all new cancer cases in adults (aged 30 years and older after the 10-year lag period) could be attributed to high BMI. Population attributable fractions (PAFs) were 5.4% (345,000) for women versus 1.9% (136,000) for men. Post-menopausal breast, endometrial, and colon cancers accounted for almost three-quarters of the obesity-related cancer burden in women (almost 250,000 cases); while in men colon and kidney cancers accounted for more than two-thirds of all obesity-related cancer (nearly 90,000 cases).
In countries with a high human development index (HDI), around 8% of cancers in women and 3% in men were associated with excess bodyweight, compared with just 1.5% of cancers in women and about 0.3% of cancers in men in low HDI countries. In a ‘counterfactual scenario’, investigators calculated that if BMI had remained as recorded in 1982, 118,000 cases of high BMI-related cancers could have been averted.
“These findings emphasise the need for a global effort to abate the increasing numbers of people with high BMI. Assuming that the association between high BMI and cancer is causal, the continuation of current patterns of population weight gain will lead to continuing increases in the future burden of cancer,” conclude the investigators.
In an accompanying commentary, Benjamin Cairns, from Oxford University, notes that “resources targeted at obesity must be balanced against those for other important causes of cancer, particularly infections and tobacco use, which are each associated with much larger proportions of cases.”
- M Arnold, N Pandeya, G Byrnes et al. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol January 2015. 16: 36–46
- B Cairns. Cancer and high body-mass index: global burden, global effort? ibidpp 3–4
Information provision should be adjusted to the individual patient
=> Cancer Nursing
Depressive and anxiety symptoms among cancer patients are associated with lower satisfaction with received patient information and perceived helpfulness of that information, finds a secondary analysis of several large population-based surveys of survivors of lymphoma, multiple myeloma and endometrial and colorectal cancers. Depressive symptoms, the Dutch investigators showed, were associated with less internet use.
Providing appropriate information can result in cancer patients experiencing a better sense of control over disease and healthrelated quality of life, and making informed treatment decisions. Many cancer patients, however, report dissatisfaction with information, resulting from healthcare professionals misunderstanding individual needs. Too much information, too little information, or too complex information may be supplied. Relationships between information provision and depression can be bidirectional: inappropriate information provision can make cancer patients feel more depressed and anxious; while in patients who are already depressed and/or anxious, perception of information can be hindered.
In the study, Olga Husson and colleagues, from Tilburg University, the Netherlands, set out to investigate whether there were associations between anxiety and depressive symptoms in cancer survivors and satisfaction with information provision and internet use. For the study 4,446 survivors registered in the Eindhoven Cancer Registry, diagnosed with endometrial or colorectal cancer between 1998 and 2007 and lymphoma or multiple myeloma between 1999 and 2008, were sent questionnaires including the 25-item EORTC Quality of Life Group Information questionnaire and the Hospital Anxiety and Depression Scale questionnaire. In total 3,080 patients (69%) responded, who were then categorised into four groups: no anxious or depressive symptoms (n=1513), depressive symptoms only (n=587), anxiety symptoms only (n=636), and both anxiety and depressive symptoms (n=344.)
Using multivariate logistic regression analyses, in comparison to cancer patients without depressive or anxiety symptoms, those with anxiety symptoms were 30% less likely to perceive information as helpful (OR 0.7; 95%CI 0.5–0.9; P<0.05); while those with depressive symptoms were 50% less likely (OR 0.5; 95%CI 0.4–0.7; P<0.001); and those with both were 60% less likely (OR 0.4; 95%CI 0.4–0.7; P<0.001). Additionally, having depressive symptoms was negatively associated with disease-related internet use (OR 0.69; 95%CI 0.5–0.9).
“The results may indicate that information provision is suboptimal, either because it is not adjusted to the mental health status of cancer patients or because it is unsatisfactory and thereby causing anxious and depressive symptoms among cancer patients,” write the authors.
For better mental health, greater attention should be paid to optimally adjust information provision to the individual patient and to check their understanding. “It is necessary to regularly check what the patient has understood and whether the information was helpful. When necessary, the HCP [healthcare professional] must repeat the information several times, both between and within consultations.”
Future studies, they add, should investigate on which subjects cancer patients want more or less information.
- N Beekers, O Husson, F Mols et al. Symptoms of anxiety and depression are associated with satisfaction with information provision and internet use among 3080 cancer survivors. Cancer Nursingpublished online 14 September 2015, doi:10.1097/NCC.0000000000000184
Comorbidities are a key driver in chemotherapy modification
=> British Journal of Cancer
Many older patients did not complete chemotherapy courses as planned, due to low-grade toxicities, a UK observational cohort study has found. Treatment modification and discontinuation for low-grade toxicity occurred more often among those with multiple comorbidities.
Delivering chemotherapy to older people can be challenging for clinicians, who need to evaluate which patients are robust enough to tolerate chemotherapy and/or continue treatment without modifications. The lack of older people in clinical trials has made it harder to make evidence-based decisions around management of chemotherapy in such patients. There are often concerns of increased risk of toxicity in older patients, with some studies indicating increased toxicity with age. Many studies, however, did not control for comorbidities, which may equally affect tolerance to chemotherapy, raising concerns that comorbidity rather than age is the contributing risk factor.
In the current study Tania Kalsi and colleagues, from Guys & St Thomas’ NHS Foundation Trust, London, set out to investigate which level of toxicity triggers treatment modification and early discontinuation of chemotherapy in older patients. Between October 2010 and July 2012, 108 patients aged 65 to 86 years (median age 72 years) were recruited from the oncology and chemotherapy clinic lists. Chemotherapy was palliative in 59.3% of them (64/108) and curative/ neoadjuvant/adjuvant in 40.7% (44/108), with 47 different chemotherapy regimens administered, 16.7% of which involved concomitant radiotherapy.
Results showed that treatment modifications due to toxicity occurred in 60 patients (55.6%), of whom 35% (21/60) had no greater than grade 2 toxicity. Early treatment discontinuation because of toxicity occurred in 23 patients (21.3%), of whom 39.1% (9/23) had no greater than grade 2 toxicity. Treatment modification for low-grade toxicity occurred in 24.4% of patients with fewer than four comorbidities compared to 57.9% of patients with more than four comorbidities, while treatment discontinuation for low-grade toxicity occurred in 33.3% of patients with fewer than four comorbidities, compared to 50% of those with more than four comorbidities. The most common low-grade toxicity types resulting in treatment modification were fatigue (n=8), haematological (n=8), gastrointestinal (n=6) and infections (n=5).
“This study would thus support that treatment decision-making should not be driven by chronological age and that comorbid burden appears far more relevant,” conclude the authors.
The findings, they add, have potentially significant clinical implications, including highlighting that the measure and reporting of lower-grade toxicity and its impact should be considered in the design of future clinical trials, especially low-grade fatigue and haematological toxicity. “This would better reflect real-life clinical decision-making and would assist clinicians in making evidencebased decisions regarding the risks of a particular chemotherapy,” write the authors.
Further work, they add, is required to clarify whether low-grade toxicity has a greater clinical impact in older patients, or whether clinicians have a lower threshold for modifying/discontinuing treatment.
- T Kalsi, G Babic-Illman, P Field et al. The impact of low-grade toxicity in older people with cancer undergoing chemotherapy. Br J Cancer 9 December 2014, 111: 2224–28
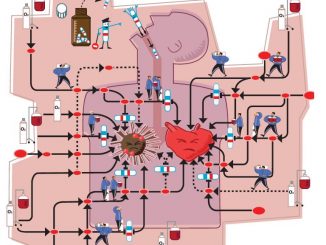
Spironolactone protects against anthracyclineinduced cardiotoxicity
=> European Journal of Heart Failure
Spironolactone administered simultaneously with anthracycline chemotherapy protects both myocardial systolic and diastolic functions, a study by Turkish cardiologists has found.
Anthracyclines represent the cornerstone in treatment of numerous haematological and solid cancers; however, the side effect of cardiotoxicity can limit use and increase rates of mortality and morbidity. While the protective effects of beta-blockers, ACE inhibitors, and ARBs on anthracycline cardiotoxicity have already been demonstrated, the effect of aldosterone antagonism, which inhibits the last step of the renin–angiotensin–aldosterone system (RAAS), has been questioned. In the current study Mahmut Akpek and colleagues, from University School of Medicine, Kayseri, Turkey, set out to investigate whether spironolactone protects the heart against anthracycline-induced cardiotoxicity.
Between September 2011 and October 2012, 83 patients with breast cancer treated with anthracyclines were randomised to 25 mg/day spironolactone (n=43) or placebo (n=40), with administration commencing one week before the start of chemotherapy and ending three weeks after the end of the chemotherapy. The choice of chemotherapy regimen was left to the discretion of the medical oncologist. For each patient, transthoracic echocardiography (TTE) was performed one week before the start of chemotherapy and three weeks after the end of chemotherapy, with patients also monitored for electrolyte imbalances every two to three weeks.
Results for the spironolactone group showed left ventricular ejection fraction (LVEF) decreased from 67.0±6.1 to 65.7±7.4 (P=0.094), while in the control group it decreased from 67.7±6.3 to 53.6±6.8. The decrease in LVEF in the control group was significantly higher than that in the spironolactone group (P<0.001). For the control group there was a significant positive correlation between total dose of anthracycline and LVEF deterioration (epirubicin r=0.655, P=0.001; adriamycin r=0.717, P=0.001). For left ventricular end-systolic diameter (LVESD), the P-value for the interaction between the spironolactone and placebo groups was 0.001; while for left ventricular end diastolic diameter (LVEDD) the P-value was 0.002. In respect of cardiac biomarkers, the P-value for the interaction between the groups was 0.018 for creatine kinase MB levels, 0.006 for troponin I and 0.130 for NTproBNP.
The study, write the authors, has three major findings. First, spironolactone protects LV systolic functions against the adverse effects of anthracycline group chemotherapeutics (not only LVEF but also LV systolic and diastolic diameters were protected by spironolactone). Secondly, spironolactone showed an antioxidant effect against anthracycline-induced oxidative stress, and thirdly it protects the diastolic functional grade against anthracyclines. “Therefore, spironolactone can be a reliable treatment option in the protection against anthracycline-related cardiotoxicity,” conclude the authors.
- M Akpek, I Ozdogru, O Sahin et al. Protective effects of spironolactone against anthracyclineinduced cardiomyopathy. Eur J Heart FailureJanuary 2015, 17:81–89