Most solid tumours will prove fatal if they are not treated with surgery and/or radiotherapy and medical therapies. But evidence is building to show that treating the primary may raise the risk of metastatic spread. Sophie Fessl looks at the evidence and the implications.
Even after treatment, patients with seemingly locoregionally defined solid tumours frequently die from metastases that may only appear several years down the line. These may arise from so-called micrometastases – clinically undetectable remote tumour growths that formed even before treatment began. Or they may arise after treatment, in cases where the treatment failed to control the primary tumour. But clinicians and researchers have been aware for some time now of a third, somewhat paradoxical, possibility: that cancer therapy, intended to treat and cure the disease, may set in motion a cascade of events in the patient that supports the formation of distant metastases. As the evidence for this process extends from surgery to include other types of therapy, questions are beginning to be asked about just how much of a danger is posed by this process, and what can be done to mitigate the risks.
 Circulating tumour cells (CTCs) have been used as a prognostic factor in different cancer types, indicating a correlation between tumour cells in the bloodstream and disease progression. In cancer surgery, evidence points to CTCs as potentially causative factors in metastasis: surgical interventions have been reported to be linked to an increase in CTCs, and levels of CTCs during an operation can predict the likelihood of disease recurrence. Tumours can, rarely, form along the needle track left during biopsy. Changes in technique during and surrounding surgery are even being implemented to reduce the risk of metastases forming.
Circulating tumour cells (CTCs) have been used as a prognostic factor in different cancer types, indicating a correlation between tumour cells in the bloodstream and disease progression. In cancer surgery, evidence points to CTCs as potentially causative factors in metastasis: surgical interventions have been reported to be linked to an increase in CTCs, and levels of CTCs during an operation can predict the likelihood of disease recurrence. Tumours can, rarely, form along the needle track left during biopsy. Changes in technique during and surrounding surgery are even being implemented to reduce the risk of metastases forming.
But a causative link between CTCs and cancer therapy may not be limited just to surgery. Research led by Michael MacManus, a radiation oncologist at the Peter MacCallum Cancer Centre in Victoria, Australia, has shown that radiotherapy in patients with non-small-cell lung cancer can mobilise CTCs. MacManus explains the rationale behind the study. “We wondered: What happens to the cellular debris when radiotherapy rapidly kills off a large tumour? As large numbers of cells may flood the lymphatic system during a course of radiotherapy, might tumour cells spill over into the circulation? To our great surprise, in our study we found that radiation therapy in non-small-cell lung cancer patients can indeed mobilise viable tumour cells into the circulation. We were the first to show that this mobilisation can occur during a course of radiotherapy.”
Radiotherapy can promote circulating tumour cells
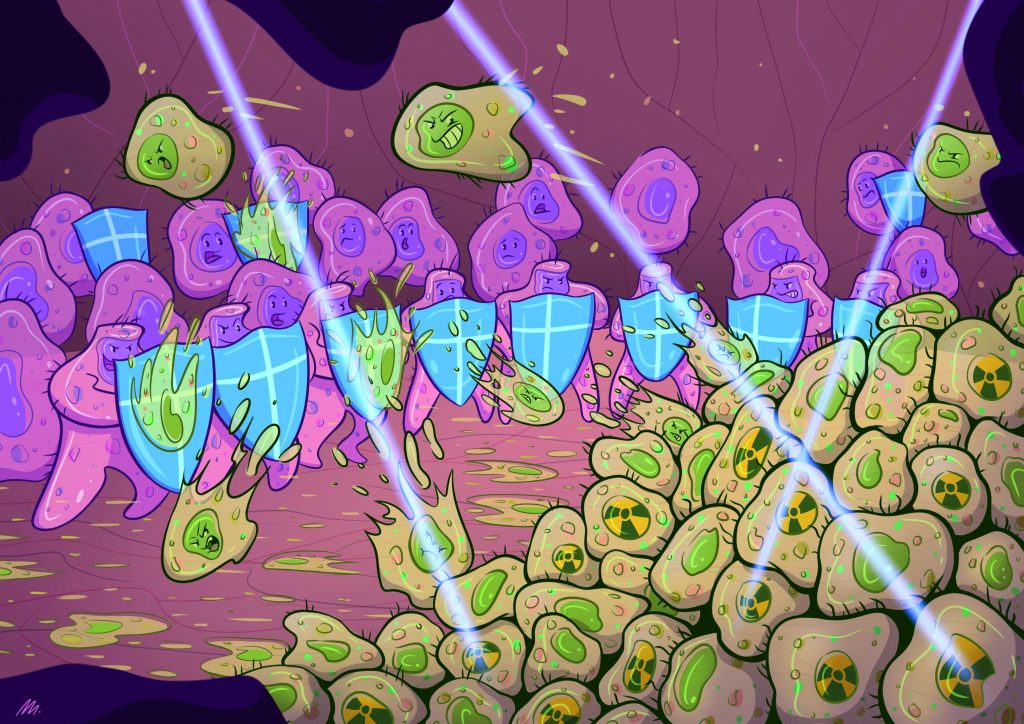
In a recent review on how therapeutic interventions might affect the risk of metastasis through circulating tumour cells (Nat Rev Clin Oncol 2017, 14:32–44), MacManus proposes several ways in which radiotherapy may enable tumour cells to acquire properties that allow them to spread more easily and subsequently form metastases. In the later phase of fractionated radiotherapy, if treatment is successful, the high cumulative dose of radiation means that tumour cells cannot reproduce any more. But in the early stages of radiotherapy, up to one half of irradiated tumour cells survive and may escape to the circulation.
This may happen through the impact of the radiation in disrupting the tumour architecture, leading to tumour cells entering the circulation either directly into the draining veins, or indirectly via the lymphatic system.
Preclinical studies show that radiotherapy can make irradiated tumour cells more aggressive than non-treated cells. In animal models, changes in gene regulation in irradiated cells are seen in genes associated with radioresistance, tumour aggressiveness, hypoxia, motility, invasiveness and epithelial-to-mesenchymal transition. Radiotherapy can also stimulate the irradiated primary tumour to self-seed from CTCs. It may also modulate angiogenesis, and so indirectly affect metastasis.
So far, the only clinical evidence directly indicating that localised radiotherapy mobilises CTCs comes from the study by MacManus and colleagues, which reported increased numbers of CTCs, both singly and in clusters, in the bloodstream of patients with non-small-cell lung cancer early in the course of radiotherapy. These mobilised CTCs were better able to grow in culture, a characteristic that can be associated with worse patient outcomes. However, there is no evidence for a direct link between radiotherapy-induced CTCs and a worse patient prognosis.
Surgery and inflammation as factors for metastasis
While the potential for radiotherapy to mobilise viable tumour cells into the circulation came as a surprise to MacManus and colleagues, evidence for a similar phenomenon occurring in relation to surgical treatment has been known about for some time. In animal models, experiments show that removing a tumour is followed by accelerated tumour growth, both at the local tumour site and at distant sites. Clinical evidence that surgery can increase both the establishment of new metastases and the growth of micrometastases is mounting. “Surgeons are aware of potential links between surgical procedures and metastasis,” says MacManus, “and are implementing changes to operating techniques to make metastasis less likely.”
Understanding more about the mechanisms that could link cancer surgery with CTCs and metastasis is a special interest of Allan Tsung, a surgical oncologist at the University of Pittsburgh School of Medicine, who co-authored a recent review on cancer surgery as a trigger for metastasis (Cancer Res 2017, 77: 1548–52). “The inflammatory response to surgery may play an important role in enhancing the risk of tumour recurrence,” argues Tsung, adding that “patients with bigger operations and those who suffer from complications and infections, have, stage-by-stage, a worse prognosis.”
In their review, Tsung et al. point to studies showing that manipulation and handling of the tumour during surgery can lead to a release of tumour cells into the circulation, and that the level of CTCs before and during an operation is a strong predictor of whether disease recurs. Inflammation and trauma, they argue, may provide an ideal environment both for capturing CTCs and promoting their growth. This point is also highlighted by MacManus et al., who describe how, after surgery, the surgical bed contains not only tumour cells, but also blood, extracellular fluid, inflammatory cells and cytokines, and suggest that this may promote the entry of CTCs into lymphatic vessels and the peripheral circulation (Nat Rev Clin Oncol 2017, 14:32–44).
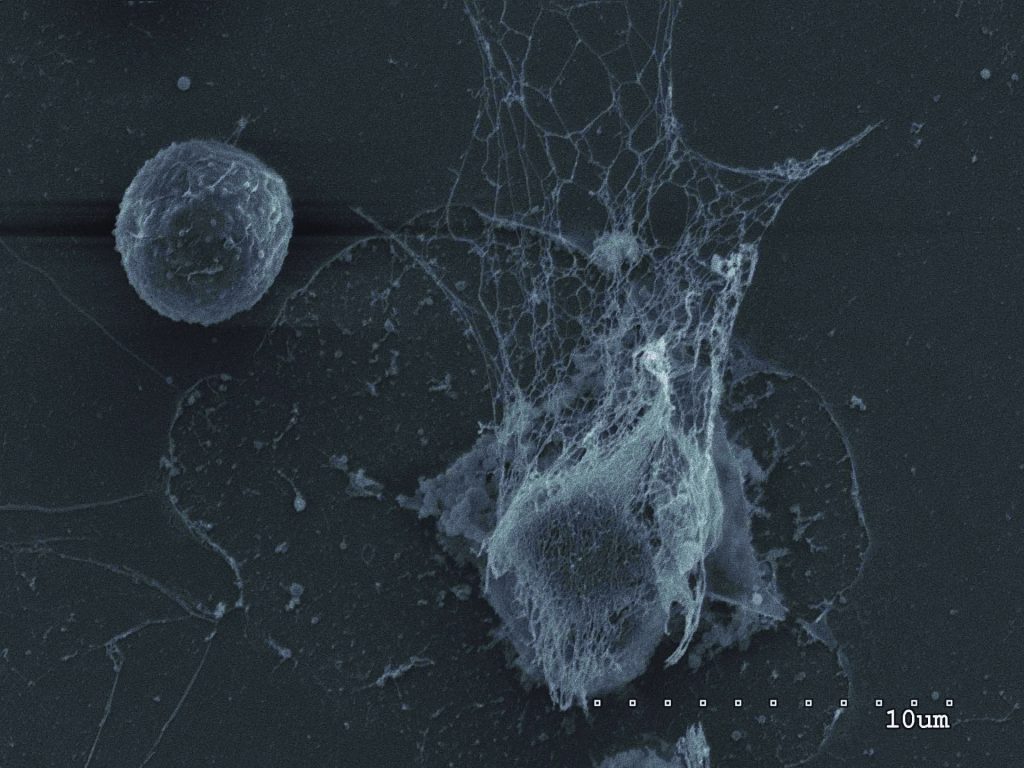
The cascade of inflammation even has the potential to capture cancer cells and promote their growth, argue Tsung and colleagues in their paper, pointing in particular to the role played by neutrophil extracellular traps (NETs) – extrusions of DNA coated with pro-inflammatory proteins that are spewed out by neutrophils in injured tissues.
After surgery, the number of neutrophils and NETs in the blood increases. NETs can capture bacteria and promote their killing, but they have also been shown to trap CTCs, says Tsung. “Through NETs, the circulating tumour cell gets a foothold in the blood vessel barrier, allowing its invasion.” In their review paper, Tsung et al. highlight a study showing that, in patients whose colorectal metastases to the liver have been surgically removed, the greater the evidence of NETs forming in the serum, the higher the risk of disease recurrence. Inflammation may also play a role in the growth of micrometastases, Tsung believes. “Inflammation after surgery may augment occult disease, so that initially dormant tumour cells grow after surgery,” he says.
Radiofrequency ablation and CTCs
A group of researchers from the departments of thoracic radiology and thoracic surgery at the Harefield Hospital in London report that the use of radiofrequency ablation can also lead to an immediate increase in CTCs (Anticancer Res 2015, 35:2823–6). Radiofrequency ablation, which uses heat generated by an electrical current to kill cancer cells, is increasingly used as an alternative to surgery in patients with surgically unresectable lung tumours. The study, by Dimple Chudasama and colleagues, measured CTCs in blood samples taken before and immediately after treatment with radiofrequency ablation in a series of nine patients. They report a general increase in CTCs in seven of the nine, noting that the largest increases were found among patients with metastatic disease, and they call for further studies to investigate the implications.
What about systemic therapies?
Clinical evidence linking systemic anti-tumour therapies with a potential for inducing metastases is lacking. However, preclinical evidence does suggest such a link could be worth investigating, in particular as part of efforts to understand why some systemic cancer treatments do not lead to the results expected.
Anti-angiogenic therapies are a case in point. This class of therapy aims to block the growth of blood vessels the tumour needs in order to survive, but its impact in patients has not lived up to the hopes and expectations initially held by many in the oncology community. John Ebos, Assistant Professor of Oncology at Roswell Park Cancer Institute, thinks that unintended effects of this class of treatment, including inducing metastases, may be part of the explanation. “Based on initial preclinical studies, it is somewhat surprising that the treatment response with antiangiogenic agents is so limited in patients,” he comments. “However, further studies in mice have generated some provocative hypotheses, and based on these further studies, this limited response is not necessarily unexpected.”
“Although inhibition of angiogenesis reduces the growth of the primary tumour, it can also promote invasion and metastasis”
Two such preclinical studies, including one led by Ebos, have shown that, although inhibition of angiogenesis reduces the growth of the primary tumour, it can also promote invasion and metastasis by inducing a hypoxic environment in the residual tumour mass. In the wake of these studies, members of the board of the Metastasis Research Society wrote an open letter to the (US) FDA and other regulatory agencies, calling for preclinical drug development to consider a cancer drug’s impact on metastasis (Clin Cancer Res 2009, 15:4529).
Other systemic therapies shown to promote metastasis in preclinical models include the BRAF inhibitor vemurafenib and cytotoxic chemotherapy agents such as cyclophosphamide. Animal models have clear limitations, however. The apparent pro-metastatic effects of some anti-angiogenic treatments in experimental systems are controversial, and probably depend on variables such as dose, the tumour system and the specific inhibitors used.
As MacManus points out, “These are very artificial models, and we do not know how to extrapolate to humans.” Ebos argues, however, that these models do have a value in studying the mechanisms of treatment-induced metastasis. “We need to make preclinical models relevant to patients. Studies in mice have uncovered biological phenomena, such as treatment-induced metastasis, that are otherwise very difficult to observe in humans.”
Clinical implications
If disturbing a tumour and its environment – particularly through surgery and radiotherapy – might, under some circumstances, promote metastasis, what impact if any should this have on clinical decision making? Does it tip the scales of benefits and risks that guide if, when and how to intervene?
Probably not, according to the current consensus. All interviewed experts agree that current standard of care therapies remain the best way to treat cancer. “This is not a reason to be worried. Cancer treatments allow many patients who would otherwise die from progressive disease to be cured,” MacManus emphasises. “It has not been proven that the mobilisation of CTCs by therapy actually causes metastasis. We need more studies to see if tumour cells circulating after cancer therapy are an important factor determining patient outcome – or if it is just a scientific curiosity. But it is a subject worth studying, and we need more clinical studies looking at how the different parameters of treatment affect patient outcome.”
Treatment-induced metastasis may, he feels, turn out to be rather similar to toxicity: an unwanted side effect that hampers the efficacy of an otherwise good therapy. Like toxicity, treatment-induced metastasis could then be taken into account when developing or choosing therapies.
One of the hopes, says Ebos, is that studying treatment-induced metastasis may ultimately improve existing therapies: “The strong benefits of cancer therapy may actually be reduced by reactive mechanisms that permit metastatic growth. Taking this into account, if we can limit this effect, we might take a good therapy and make it great.”
“Studying treatment- induced metastasis may enable us to take a good therapy and make it great”
Steps to improve therapy in the light of potential treatment-induced metastasis have already been taken in cancer surgery, says Tsung, including using keyhole surgery to limit the trauma. More direct measures are also used, he adds. “Small trials have shown us that using agents to block the inflammatory response affects cancer development. Deoxyribonuclease, which is used for treating cystic fibrosis, could be used to inhibit NETs after tumour surgery.” Attention is also paid to factors around surgery, such as the anaesthetic agents used, which may alter aspects of the immune response and affect tumour spread.
If MacManus’ finding that radiotherapy releases CTCs indeed has prognostic value, he suggests that strategies to either target CTCs or ensure that they are critically damaged before they even enter into the circulation would be appealing. “These strategies could include larger or more-frequent fractions of radiotherapy, or modulating the immune system to eliminate CTCs, among others.”
Getting the message right
How should a potential link between treatment and metastasis be communicated, both to the patient and the wider community? MacManus admits concern: “I’d hate the message to be that patients shouldn’t have conventional therapy. In reality, if a carcinoma spreads to the lymph nodes, the patient will die without surgery and/or radiotherapy. But the patient may fare better if we improve the available treatments.”
Bernhard Albrecht, a German journalist and former doctor, who has investigated the way alternative therapists promote their services to cancer patients (see, for instance, Dangerous Healers, Cancer World Nov–Dec 2015), flags up the risk that this sort of research will be abused to lure people away from evidence-based treatments. “Alternative healers have a very selective view of science, and pick out anything critical. When medicine is – rightly – self-critical, the arguments get adopted and generalised.”
Scientific arguments get distorted, says Albrecht, so that they fit into the worldview of alternative therapies. “While the intention of looking into surgery-induced metastasis is to bring this phenomenon to light and address it, a homeopath I talked to simply said: ‘See, this is how dangerous cancer surgery really is!’ No amount of corrections or reactions by the original authors of the scientific publications is able to change this misappropriation.”
“Strategies to either target CTCs or ensure that they are critically damaged before they enter into the circulation would be appealing”
There is no magic formula to stop people cherry-picking evidence in this way. It certainly should not stop researchers, clinicians and patients alike from participating in honest discussions and carrying out further research to clarify the complex relationship between cancer treatments and metastasis. Indeed pursuing this research is vitally important, argues MacManus. “If we can take a link between treatments and metastases into account in our therapies, there may be some patients that could be cured who are not cured now.”
Progressive e ects of fractionated radiotherapy on tumour cells in vivo
Up to 50% of the malignant cells in an irradiated tumour can survive the first radiotherapy fractions; they can subsequently acquire a more-aggressive phenotype, becoming circulating tumour cells that are detectable during the course of radiotherapy. Radiotherapy affects the regulation of genes associated with radioresistance, tumour aggressiveness, and enhanced metastatic potential, including signatures associated with hypoxia, invasiveness and motility, and epithelial-to-mesenchymal transition (EMT).
Source: OA Martin et al (2017) Does the mobilization of circulating tumour cells during cancer therapy cause metastasis? Nat Rev Clin Oncol 14:32–44, reprinted with permission © Macmillan Publishers Ltd